
Researchers at UHN’s Schroeder Arthritis Institute have gained significant insights into the mechanisms underlying spondyloarthritis (SpA), an inflammatory disease that affects the spine and joints.
The team identified hypoxia-inducible factor-1 alpha (HIF1A) as a key player in SpA, which promotes inflammation and other disease characteristics.
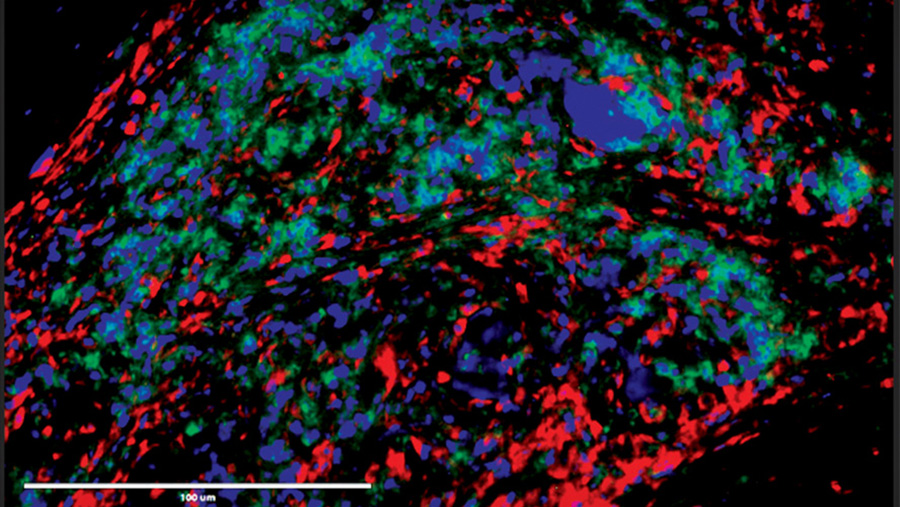
Two hallmarks of SpA are inflammation, where an overactive immune system causes pain and swelling, and new bone formation, which involves unwanted bone growth in inappropriate areas, leading to joint problems.
The current therapies for SpA provide relief in only a proportion of patients and there is no cure. Moreover, there are several therapies that have failed.
This raises the questions of what is really the cause of SpA and which major molecules are driving the disease process?
“Previous research from our lab identified a protein called macrophage migration inhibitory factor (MIF) as a driver of the disease that amplifies inflammation and new bone formation,” says Dr. Nigil Haroon, Senior Scientist at the Schroeder Arthritis Institute and senior author of the study.
“However, the mechanisms behind this and the proteins that it interacts with remained largely unknown,” says Dr. Haroon, who is also Head of the Division of Rheumatology at UHN and Sinai Health.
The research team aimed to bridge knowledge gaps in SpA disease development by identifying MIF-interacting molecules and examining the role of MIF-producing immune cells, called neutrophils, in disease progression.
“We identified HIF1A as a partner molecule physically interacting with MIF,” says Dr. Akihiro Nakamura, first author of the study and former clinical fellow in Dr. Haroon’s lab. “We found that this interaction promotes inflammation and new bone formation in SpA.”
The team discovered that HIF1A increased the production and release of MIF and an inflammatory marker called IL-23 in neutrophils. Inhibiting HIF1A with a selective inhibitor reduced the expression of MIF and IL-23 and reduced the severity of arthritis and other SpA symptoms in pre-clinical models.
They also found that increasing IL-23 levels induced SpA symptoms, while deletion of HIF1A and MIF suppressed IL-23-induced arthritis development, including new bone formation.
Overall, these results suggest a novel MIF/HIF1A regulatory network in SpA, functioning through immune response regulators such as IL-23.
This study offers significant insights into the mechanisms underlying spondyloarthritis and opens new avenues for treatment.
“These findings suggest that inhibiting HIF1A could be a novel therapeutic approach for treating SpA,” says Dr. Haroon, who is also an associate professor at the University of Toronto’s Institute of Medical Sciences. “By understanding the roles of MIF and HIF1A, we can develop targeted therapies to alleviate symptoms and slow the progression of this chronic condition, improving the quality of life for patients with SpA.”
By UHN Research Communications
This study was supported by generous donors to UHN Foundation.

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.


