Internal Medicine

Comprehensive health care
In today’s health care landscape, patients are frequently grappling with complex medical conditions requiring diagnosis of challenging symptoms, extensive care, and multi-organ conditions. For these patients, UHN’s Internal Medicine (IM) program provides comprehensive, specialized and coordinated care. Specialists throughout the UHN look to IM doctors for their wide breadth of knowledge and expertise for patients who do not yet have a unifying diagnosis or for patients with diseases beyond the scope of one medical specialty.
The typical IM patient has four to five chronic medical conditions and takes upwards of 10+ medications.
IM patients are often frail, elderly and economically disadvantaged, and a significant percentage do not speak English as a first language.

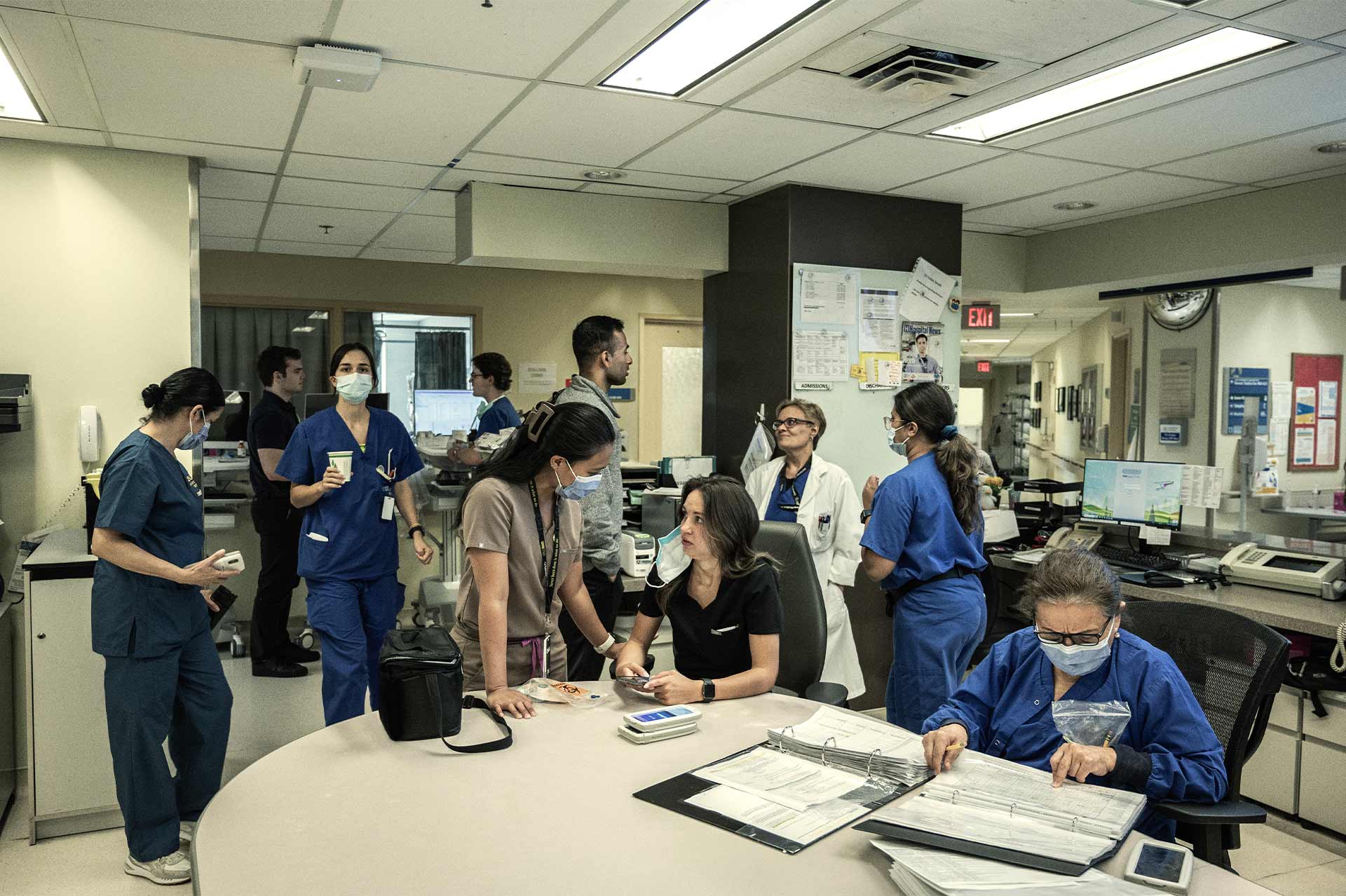
Multidisciplinary teams
The IM service is responsible for over 50% of all patients hospitalized at UHN, and the vast majority of IM cases are unplanned and come through the emergency room or as a result of 911 calls. IM patient wards are located at both Toronto General Hospital and Toronto Western Hospital and are the largest inpatient units at UHN. These wards are also the home to Clinical Teaching Units, where faculty physicians provide foundational training in all aspects of internal medicine. This critical training ensures that medical students, residents, fellows and members of multidisciplinary health care teams are skilled at caring for the whole patient with the utmost compassion and humanistic approach.
TWH Internal Medicine Clinic
Capacity: 5000 visits/year with 100 new patients/month
Top diagnoses include: high blood pressure, abdominal pain, skin/soft tissue infections
Five year vision: to be the leading centre of excellence for IM clinic care in Canada
Investments in clinic expansion would allow IM to significantly expand capacity to offload our crowded Emergency Departments and help end hallway medicine.
The IM program is the heart and soul of UHN, touching the lives of patients every day in every department. Donor support empowers and supports the Internal Medicine team as they deliver comprehensive patient care and work to identify and address emerging challenges in our health care system.
Fundraising priorities
Attracting top medical talent is key to advancing research and clinical care. Chairs, professorships and fellowships support these efforts by building specialized expertise and driving innovation.
The HoPingKong Centre for Excellence in Education & Practice fosters innovative solutions to health care challenges. Transforming the health system through research and education ensures better patient care and supports ongoing system improvements.
Focused on transforming patient care, new clinical programs, including rapid cancer diagnosis and post-discharge support, streamline processes and reduce wait times. This ensures patients receive timely, efficient care across all stages of treatment and recovery.
Infrastructure improvements will enhance IM’s clinical space and expand access through virtual appointments, e-consult services, and educational rounds, improving patient care and system efficiency.
Seed funding for innovative projects addresses critical health care issues, fostering practical solutions to improve outcomes and system efficiency.
Contact information:
Afsheen Jiwani, MBA, CFRE
Campaign Director, Major Gifts
647.502.7538
[email protected]