Imagine an operating room with a built-in MRI so surgeons have real-time imagery of a patient’s anatomy deep inside the brain during a procedure, where the latest in surgical robotics provide precision and control beyond human capability, and where doctors-in-training can observe from next door or from all the way across the globe.
This is what neurosurgery will look like at UHN’s state-of-the-art, 15-storey surgical tower currently under construction at Toronto Western Hospital. A $1.1-billion project that will add 82 private patient rooms and 20 operating rooms, the tower will boost UHN’s overall surgical capacity by up to 50 per cent.
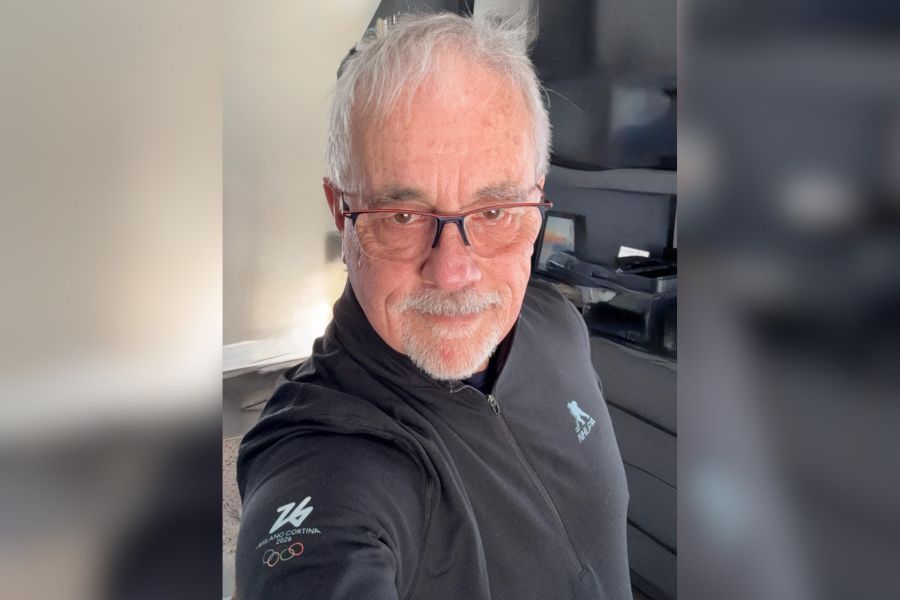
Dr. Taufik Valiante, neurosurgeon and director of the Surgical Epilepsy Program at UHN’s Sprott Department of Surgery and Krembil Brain Institute, says he’s excited about what he and his colleagues will be able to accomplish in the new tower.
“We’re not only providing treatment [at UHN], we are learning about the brain,” says Dr. Valiante. “We see UHN and this tower becoming a focal point for human brain science. As neurosurgeons, we not only try to deliver the best possible care we can, but we also take those unique opportunities where patients allow us to push the science forward.”

Transforming care of neurological disorders
UHN’s Sprott Department of Surgery is the largest surgical program in Canada, handling the most complex surgical cases in the country.
The new surgical tower will be the home for the innovative work of the likes of Dr. Valiante and his colleague Dr. Suneil Kalia, a neurosurgeon in UHN’s Sprott Department of Surgery and Krembil Brain Institute and a Parkinson’s disease specialist. Both are leaders in their fields specializing in neuromodulation, a method of adjusting or correcting dysfunctional brain circuits by stimulating neural pathways.
Dr. Kalia says that the advanced technology that will be housed in the surgical tower will be a “major step forward” for the work he and Dr. Valiante are doing at UHN, which is home to the country’s largest neuromodulation program.
Deep brain stimulation – which involves inserting electrodes as thin as one millimetre into the brain or spinal cord – is one form of neuromodulation, used to reduce symptoms in patients with chronic pain, epilepsy, movement disorders like Parkinson’s disease, depression and substance abuse disorders.
The built-in imaging equipment in the operation rooms will improve the targeting and safety of the deep brain stimulation procedures, Dr. Kalia says.
“If we are delivering a treatment such as electrodes into the brain, we can visualize it in real-time,” he says. “We will have the opportunity to do operations with the latest technology that we’ve not yet been able to do, to date.”
More capacity to meet a growing need
Drs. Valiante and Kalia point out that there is a pressing need for the new facility since more than 10 million Canadians live with neurological or mental health conditions. Globally, brain disorders account for more than 25 per cent of the total disease burden, more than heart disease and cancer combined.
“The capacity is being built to serve the growing and aging population,” says Dr. Valiante. Indeed, diseases such as Alzheimer’s and Parkinson’s are growing rapidly in Canada as the population ages. For example, Parkinson Canada predicts that 150,000 people will be living with Parkinson’s disease by 2034.
In addition to treating patients, the new surgical tower will become an important driver of research and training by placing labs and learning environments next to operating rooms.
“This space will facilitate our teams to develop the next generation of treatments for the brain,” says Dr. Kalia. “We’re moving from the operating room to the research bench, and then back to the operating room.”
In essence, operating rooms will become “living labs” where the next breakthrough in neurological treatment and care could be developed.
“Young minds, who are getting introduced to neuromodulation at the university level, can come before in to see the things that are done, and contribute, not only from a scientific point of view, but from an innovation perspective,” adds Dr. Valiante. “This new space will allow us to do that on a scale that we can’t do right now.”
Operating rooms will also be equipped with telesimulation technology – surgical simulators, cameras and internet connectivity – enabling surgeons at UHN to train medical professionals in remote communities and around the world.

Donor support is ‘mission critical’
The new surgical tower is slated to be up and running by 2028, but community support is key to bringing the tower to life.
“Donor funding has allowed us to push science in a way that traditional funding models do not,” Dr. Valiante explains.
Dr. Kalia says the need for adequate funding is “mission critical” to remain leaders in the fields of neurosurgery and neuromodulation.
“Philanthropy allows us to recruit the best people to our team and have access to the best and latest technology,” he says. “That’s how we’re going to continue to innovate and push the field. This is important for Canada.”
To learn more about supporting UHN’s surgical tower project, go to uhnsurgicaltower.ca.
This article originally appeared in The Globe and Mail.


No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.