By Anna Sharratt
Long before most people wake up, the Sprott Department of Surgery’s team of nurses, nursing attendants and anesthesia assistants is hard at work creating as safe an environment as possible. They’ve checked their patients’ identities and vitals, and assessed their anesthesia needs. Some will have met with specialists to manage additional health conditions. Others have diligently prepared the operating room (OR), discussed the procedure with the surgeons and briefed the post-surgical team. Most importantly, they’ve devoted a large part of their day to reassuring and comforting their patients.
It takes a small army of professionals to pave the way for all of the groundbreaking surgical procedures that happen at University Health Network (UHN). With a commitment to personalized care, they ensure a patient’s surgical journey is as worry-free as possible, clearing the way for a complication-free recovery. Many people make Sprott Surgery tick, but here are four key players setting up the OR, and its surgeons and patients, for success.
The mastermind: Clare Attley
Patient Care Coordinator, cardiac and vascular ORs, Sprott Department of Surgery
If anyone knows the inner workings of Sprott Surgery, it’s Clare Attley, who has spent 42 years at UHN and has, by her estimate, seen more than 20,000 patients. “Even after four decades, I come to work and hope that, as a team, we can make a difference in people’s lives,” she says. The Patient Care Coordinator helps oversee six cardiac and vascular ORs and, with the OR Clinical Manager and three other patient care coordinators, leads a team of 120 nurses, ensuring they’re prepped for the surgeries they’re involved in.
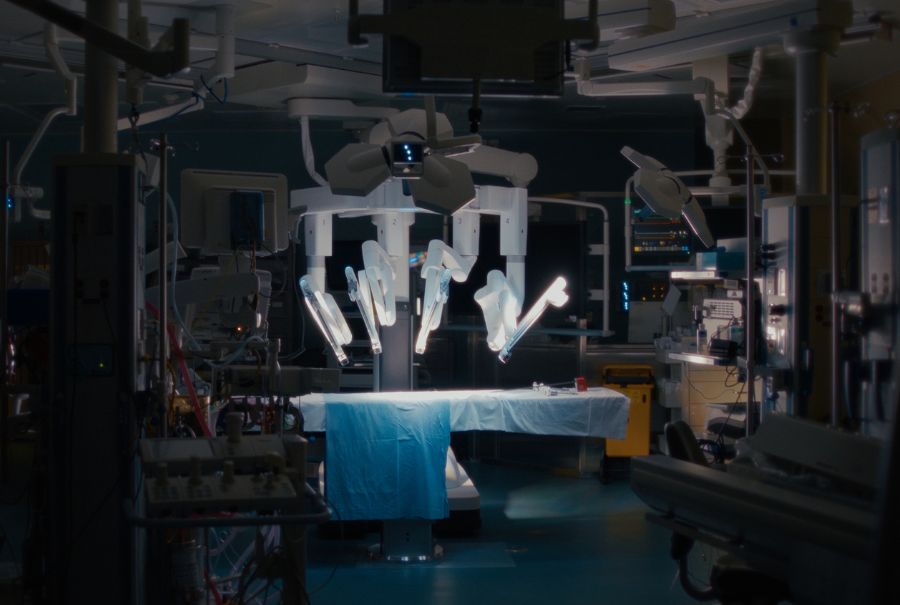
Attley used to be a scrub nurse in the OR, but she’s since turned her attention to implementing several innovative programs at Sprott Surgery. For instance, she’s played an integral role in creating a cardiac-focused minimally invasive surgery program at UHN during the pandemic. “Patients want to have less invasive procedures,” she says. “If they’re the right candidates for this type of surgery, they can be in the hospital for less time, have shortened anesthetic times and don’t need to be hooked up to a heart-lung machine during heart surgery.”
The original plan was to send nurses to train in Germany, where one of Sprott Surgery’s minimally invasive surgery surgeons came from, but that trip was cancelled due to COVID-19. Instead, she set up training at UHN, while at the same time having to figure out how to order key instruments during supply chain-challenged times. “The learning curve was steep,” she says about the program.
More broadly, when it comes to keeping ORs running smoothly, Attley goes above and beyond, ensuring everyone is where they need to be at all times. “I have to keep everyone happy,” she laughs. Attley’s biggest source of pride, however, is how her team pulls together when surgical patients arrive. “We have the best team here – everyone pitches in when a patient is in dire circumstances,” she says. “It means everyone is doing their best to save a person’s life.”

The troubleshooter: Romeo Cruz
Clinical Nurse Specialist, Sprott Department of Surgery
Many of Romeo Cruz’s patients struggle with physical and mental health issues. They have swallowing and eating issues related to tumours or are dealing with side-effects, such as nausea or mouth and throat swelling, from radiation or chemotherapy. “I have to make sure they are fit and ready for surgery,” says the Clinical Nurse Specialist in Sprott Surgery’s Head and Neck Inpatient Unit.
Cruz spends most of his days working with head and neck cancer patients, who are preparing for mouth, larynx, thyroid or salivary gland surgeries. Many have other medical conditions, such as coronary heart disease, chronic obstructive pulmonary disorder and diabetes, which must be addressed before surgery. Timelines are often tight, with surgeries happening just weeks after an initial consultation. “The turnaround for surgery is so small,” he says, adding that he has to work quickly to consult with clinicians about care plans or arrange pre-op services for the patient.
The 21-year UHN veteran must also liaise with nutritionists and dietitians to address nutritional issues and meet with patients’ families to help them understand the plan of care.
After surgery, Cruz follows up with patients, arranging for home care and hospital visits. “I have to ensure a seamless transition between episodes of care,” says Cruz. “The best part is knowing that you’re helping patients go through this as safely and comfortably as possible.”

The early bird: Nejaha Abubeker
OR Attendant, Sprott Department of Surgery
Every morning at 3:30 a.m., a bleary-eyed Nejaha Abubeker gets out of bed, turns on the coffee maker and gets ready for work. The OR attendant rides the mostly empty bus to the hospital, arriving an hour and a half before most of her co-workers walk through the door. Her job? Setting up the OR for a busy day of surgeries. “I love that early shift because I can go at my pace,” she says. “I’m setting up the rooms with IVs, blood, blood warmers and tools.”
Once she’s prepped her ORs, most of which perform cardiac, ear, nose and throat, or general surgeries, she escorts the surgical patients to their procedures. “I greet them, make sure I check their arm bands and ensure I am getting the right patient to the right room,” she says.
Part of her job is also to calm down and relax anxious patients, which she does by telling them amusing stories about her five children. “I’m here to help the patient,” she says, adding that she takes time to answer any questions a patient might have and put their mind at ease. Her methods work. “I’ve never had a panicking patient I couldn’t calm down,” she says. After the surgery is done, Abubeker meticulously cleans the OR and brings in any extra equipment needed for the next procedure.
Abubeker’s days, which usually end around 2:30 p.m., may be jam-packed, but she says it’s special working alongside a closely knit team. “My fellow OR attendants and the nurses, managers and surgeons are like family,” she says. “It’s busy, but I love it.”
The trailblazer: Rajesh Patel

Charge Anesthesia Assistant, Toronto Western Hospital, Sprott Department of Surgery
Rajesh Patel knows about flexibility. The charge anesthesia assistant, who has been with UHN since 1992, is responsible for scheduling 45 anesthesia assistants at Toronto Western Hospital and Women’s College Hospital. His staff, who are specially trained registered respiratory therapists and critical care registered nurses, must move fluidly between the main ORs and other surgical divisions, as well as endoscopy, echo labs, cardiac procedure rooms and MRI units, providing coverage where needed and giving breaks to anesthesiologists.
His team’s flexibility has proven invaluable at a time when COVID-19 has created a backlog of surgeries. “UHN is leading this profession,” he says of the role, adding it has helped boost surgical efficiency. “We increased the number of surgeries we do.”
In 2001, UHN became the first centre to widely implement the role of an anesthesia assistant.
While anesthesia assistants are not anesthesiologists, they can work independently in an OR under orders from an anesthesiologist, where they can assess the patient, place IVs and administer anesthetics safely. Anesthesia assistants enable the anesthesiologists to run more complex and difficult cases, while the anesthesia assistants complete shorter and less-invasive cases. Anesthesia assistants play a vital role in the OR, and with them, UHN has been able to increase the number of surgeries performed daily.
Patel is most fond of the constant learning opportunities and challenges his position deals with. “It can be a quiet, calm day in the cataract room or a difficult one in the cardiac room,” he says. “We do so many varied and different cases. No day is the same.”
This original article appeared in the 2023 issue of the Sprott Department of Surgery magazine.

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.