In lung cancer diagnostics, there is nothing more valuable than time. The earlier a patient is diagnosed, the sooner treatment can begin.
With the support of donors to UHN Foundation, a team of UHN researchers is inventing a new tool that could get patients answers faster. It’s called EBUS-Chek, and it is the latest in a long line of UHN inventions that have transformed lung cancer diagnostics and surgical treatment for lung cancer.
UHN invention, global gold standard
Another UHN invention came first, setting the new gold standard in lung cancer diagnostics.
Dr. Kazuhiro Yasufuku, Head of the Division of Thoracic Surgery and William Coco Chair in Surgical Innovation for Lung Cancer, led the invention of the EBUS-TBNA (endobronchial ultrasound-guided transbronchial needle aspiration) procedure.
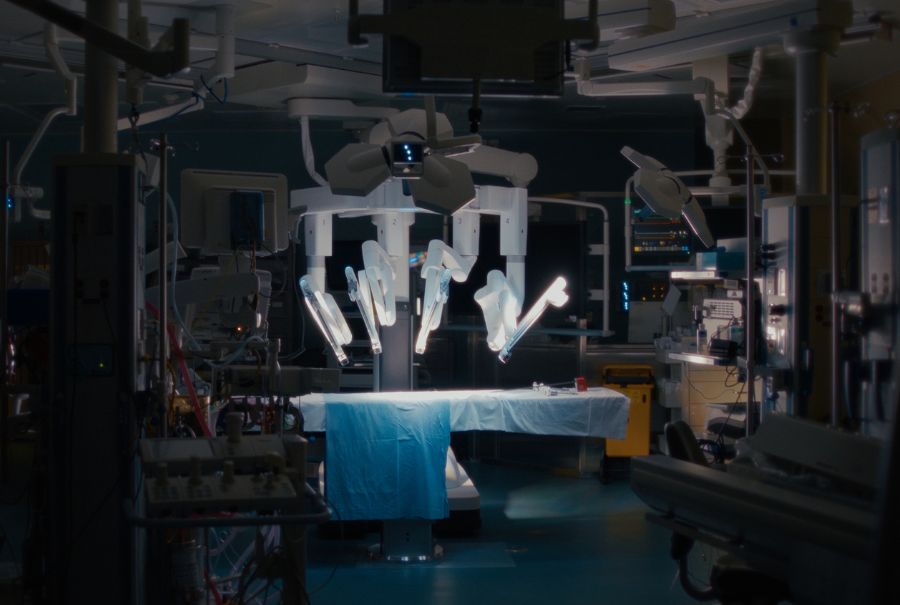
With EBUS-TBNA, surgeons steer a thin and flexible scope through a patient’s airways, guided by ultrasound images. This allows them to navigate deep into the lungs and take biopsy samples from the lymph nodes. This minimally invasive procedure allows patients to avoid undergoing surgery just to get a biopsy.
A major leap forward in lung cancer diagnostic technology, EBUS-TBNA is used in more than 3,000 hospitals around the world to stage and screen patients more effectively, with a lower risk of complications.
But the next challenge comes with processing and analyzing the biopsies themselves.
The challenge of delays in lung cancer screening
Biopsies taken with EBUS-TBNA need to be assessed to ensure they are sufficient to be used for diagnostics and staging of lung cancer. This is essential because an insufficient biopsy could lead to an incorrect diagnosis, such as a false negative result or an inaccurate staging.
The current best practice is for biopsy specimens to be assessed through Rapid On-Site Evaluation (ROSE), where a cytopathologist is present during the procedure and provides immediate feedback on the specimen. This real-time evaluation helps to reduce non-diagnostic samples, minimize repeat procedure and improve overall diagnostic accuracy and patient management. However, due to the high cost and resources required for ROSE, the vast majority of hospitals around the world do not have access to it.
This means that in some cases without ROSE, the final results of the biopsy may come back as inadequate, and the process needs to begin all over again; the patient is subjected to another biopsy, and another anxious period spent waiting to learn if the biopsy is sufficient.
These delays are heartbreaking – wasting precious time and leaving patients struggling with anxiety while they wait for answers.
Dr. Yasufuku and his team believe that there is a better way. Their latest invention underway, EBUS-Chek, might just provide the solution.
How EBUS-Chek could speed up lung cancer diagnostics
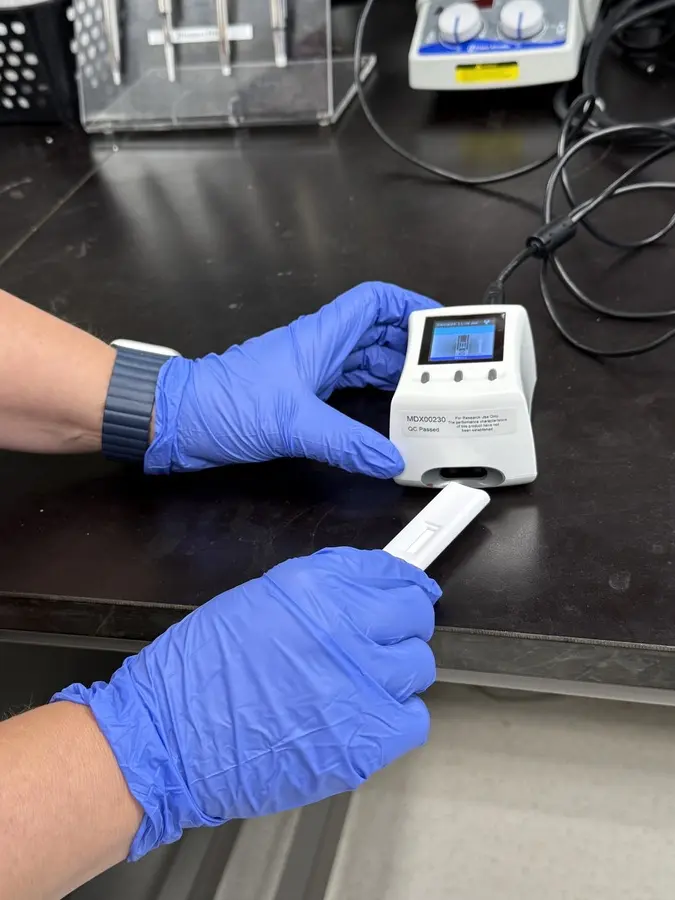
EBUS-Chek is a tool under development to rapidly test the sufficiency of lung cancer biopsies, confirming whether or not they are sufficient for diagnosis and staging.
The concept is deceptively simple. The biopsy sample is placed on a microchip, which works to detect “biomarkers” – important biological signs discovered by the team that are associated with a sufficient biopsy. Then, the readout indicates whether or not the biopsy is sufficient.
The test is designed to provide results in less than five minutes – cutting wait times down from weeks to mere minutes. This will help patients start their treatment – and undergo any needed surgical care – faster.
“It will potentially increase the diagnostic yield of lung cancer, and help clinicians in getting to that diagnosis of lung cancer,” says Dr. Yasufuku. Diagnostic yield is the proportion of cases in which a biopsy successfully provides a diagnosis.
Philanthropy powers innovation
From the initial idea through to prototype development, EBUS-Chek has been supported by donors to UHN Foundation. Dr. Yasufuku highlights the enormous impact that philanthropy has in making projects like this possible.
“Philanthropy helps us enormously because the regular granting agencies do not support new, innovative projects like this, not until you have all the data,” he says. Generating that data requires the project to already have launched, so philanthropy is needed to ensure projects like this can get started in the first place.
“With EBUS-Chek, it was especially challenging because we needed to make a prototype, and again, most grants don’t support this,” Dr. Yasufuku says. “Our donors were essential in helping us transition from bench to bedside, get to that first prototype, and perform all the research that has gone into this project.
“Without philanthropy, we would not be here,” he says.
EBUS-Chek currently continues in development, and its potential to revolutionize lung cancer screening is enormous. Technologies like these are one of the many ways UHN is transforming surgical care.

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.