Dr. Mark Osten, (L), of UHN’s Peter Munk Cardiac Centre, and Dr. Lee Benson, an interventional cardiologist at SickKids Hospital, collaborated on the Canadian-first procedure. Dr. Osten holds in his hand a 3D model of the patient’s heart, which was used to plan the surgery. (Photo: UHN)
In 2017, Robert Arias went to his family doctor asking if it was safe to return to the gym. The then-48-year-old mechanic was experiencing some occasional discomfort in his chest. He wanted to make sure it was nothing serious.
After an initial electrocardiogram, doctors as Sunnybrook Health Sciences Centre referred Robert to UHN’s Peter Munk Cardiac Centre (PMCC) where he learned he had an arterial septal defect (ASD) – a hole in his heart.
“Looking back, I knew in my gut something was wrong, but I didn’t realize how serious it was,” Robert says. “I thought I was just tired from work.”
The heart of the matter
ASDs are congenital but patients may not present with symptoms until adulthood. In some cases, very small defects can close during infancy or early childhood. Depending on the type of defect, patients can be treated through cardiac catheterization, a minimally invasive technique that goes through a vein in the groin to access and repair the heart.
While the majority of ASD repairs are done in the catheterization (cath) lab, cases like Robert’s typically require a more invasive approach.
“Usually, patients with this type of ASD called a sinus venosus defect, require open-heart surgery,” explains Dr. Mark Osten, an interventional cardiologist at PMCC. “Until recently this type of ASD couldn’t be repaired in the cath lab, at least not here in Canada.”
In 2021, open-heart surgery is considered relatively safe – the PMCC performs hundreds of surgeries via sternotomy per year – but like any surgery, it’s not risk-free. Moreover, patients typically require months to fully recover.
“I had to work. I had to put food on the table. I felt stuck,” Robert says.
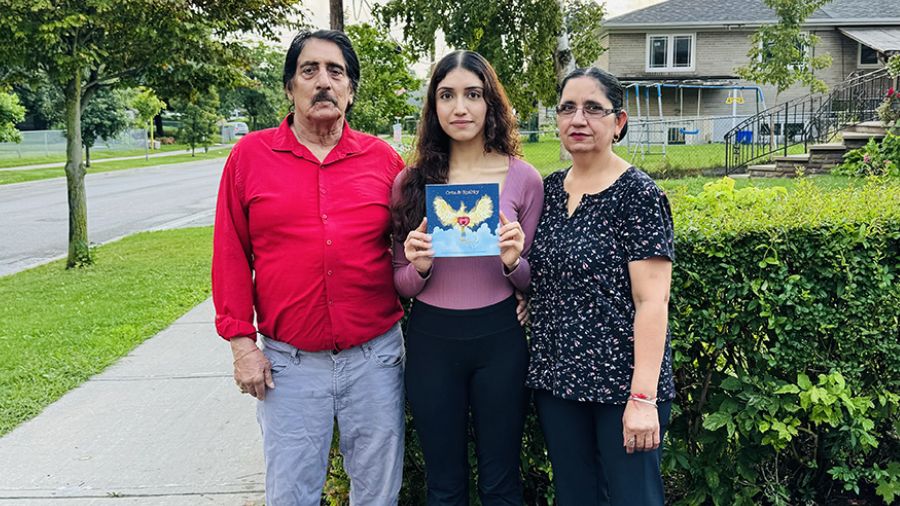
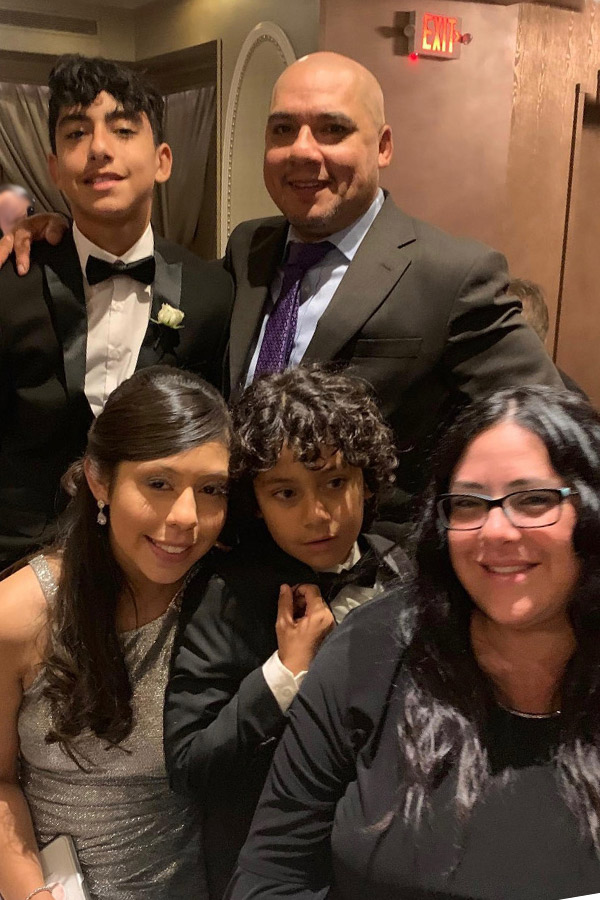
Unsure what the future held, Robert focused on his family.
“I spent a lot more time with my kids and my wife, just doing normal things, things I hadn’t prioritized before,” he says. “I wasn’t sure how long I would have with them.”
A minimally invasive solution
Dr. Osten says over the past few years experts have been trying to figure out how to do the type of repair Robert required through catherization.
“Avoiding open-heart surgery is ideal for many reasons,” he says. “Patients have a shorter hospital stay and a faster recovery than the alternative.
“They can even get back to their normal lives within a couple of days.”
Dr. Osten and his team, including Dr. Lee Benson, an interventional cardiologist at SickKids Hospital, collaborated with UHN’s 3D lab to create a model of Robert’s heart. In a matter of days, Dr. Osten was able to successfully simulate the closure on the 3D replica with a covered stent.
“Because this heart defect is relatively uncommon, device manufacturers don’t typically invest in developing a product,” Dr. Osten says. “By creating the 3D model, and simulating the implant, we developed a much deeper understanding of the anatomy, and realized we could use an available technology – used to treat other congenital heart defects – to repair sinus venosus defects.”
Robert says he “knew the conventional way (of repair) wasn’t going to work for me.
“So, when Dr. Osten pitched this idea, I was nervous but I felt like I had finally had a feasible option – and someone has to go first.”
The procedure was scheduled for January 2020 but was postponed due to COVID-19.
For months, Robert and his family waited.
“It was agonizing to know that I needed this done and it couldn’t happen right away,” he says.
“But I had a lot of faith in Dr. Osten. I knew he was going to make it happen for me.
“They were just waiting for the right time.”
A Canada first
When the time came, the turnaround was quick. After an overnight stay in hospital, Robert returned home to his family, more energetic than he had been in years.
The procedure – a Canadian first – had been a success.
“I remember when I woke up, I just sat there and listened to my heartbeat,” Robert says. “It was so smooth.
“It was like Christmas times one thousand. Everything just felt better. I couldn’t believe it.”
Thanks to the team’s pioneering efforts, led by Dr. Osten, minimally invasive repair of sinus venosus ASDs are likely to become the preferred treatment for patients in Canada. The procedure is suitable for any age, meaning that patients who present with symptoms in childhood would potentially be eligible.
Months after his brief hospital stay, Robert started his own business, something he had dreamed about for years.
“Everything happens for a reason,” he says. “This was a real wakeup call. It changed my job, my perspective, everything. I get to see my kids grow up. I’m finally my own boss. I feel so hopeful.
“Dr. Osten saved my life. I’m so grateful.”