Emergency
Transforming the patient experience in the Emergency Department
Toronto is North America’s fastest-growing city, and downtown hospitals are struggling to keep up with the demand. Even before the COVID-19 pandemic, one of the biggest challenges facing Emergency Departments came from the inability to assess and treat patients in a timely manner due to high and ever-growing patient volumes. A growing city and a global pandemic are straining them like never before.
Toronto General Hospital’s Emergency Department was designed to care for about 20,000 patients per year, but currently cares for more than 55,000. With our rapidly growing population, we anticipate an increase of more than 18,000 patients over the next five years. Due to COVID-19 distancing and contact precautions, 40 per cent of care spaces have been lost – making the need for additional space critical, now more than ever. As a result, we are expanding the Emergency Department at Toronto General Hospital. The new expansion is designed as a pandemic-ready and surge space to increase capacity by 9,000 square feet.
More about Emergency Medicine at UHN
World-class care
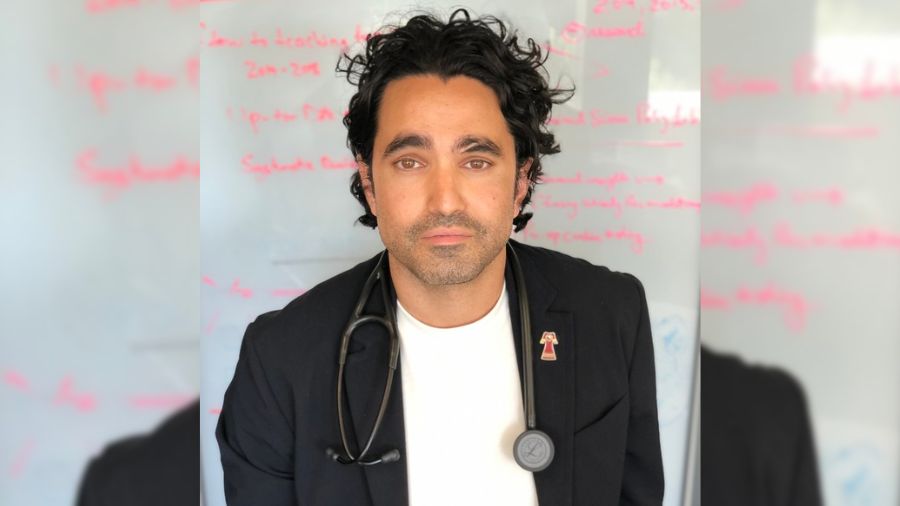
The Emergency Medicine team at UHN comprises 90-plus physicians, nurse practitioners and physician assistants, and more than 200 nurses across two sites: Toronto General Hospital and Toronto Western Hospital.
The team has the knowledge to compassionately care for the sickest and most complex patients from across Canada due to highly skilled experts and UHN’s leadership as a national referral centre.
Health care’s safety net
Emergency Departments are essential infrastructure in our community. Open every day and at every hour, they serve as the safety net of the healthcare system. Patients with social complexity, addictions and mental health diagnoses use our Emergency Departments to address both medical and social needs. More than half of these patients live in low-income neighbourhoods or lack housing. Homelessness increases the risk of contracting COVID-19. In extreme situations, patients use the department solely for needs such as food, shelter, clothing and loneliness. UHN’s Emergency Departments play a profound role in connecting patients with resources that address not only their clinical needs, but also their overall well-being.
Impact of COVID-19
UHN’s Emergency Departments were the first line of defense at the onset of the COVID-19 global pandemic, serving as two of Ontario’s initial testing centres. Some of the sickest coronavirus patients continue to come to UHN due to its leadership as the largest ECMO program in Canada and referral centre in the province. Additionally, because of the pandemic, physical distancing and infection prevention measures have reduced emergency care spaces.
We need donor support to expand the Emergency Department at Toronto General Hospital – to care for the patients who need us the most, even in the most trying of times.
Fundraising priorities
Faster. Safer. Streamlined. The new Michael Lawrence Turk Rapid Assessment Centre at Toronto General Hospital will address the challenges facing our Emergency Department and improve the patient experience, now and into the future. Expanding Emergency care space is directly linked to UHN’s ability to respond to the COVID-19 global pandemic.
The new registration process will feature two separate streams: one for very complex and sick patients, and a fast-tracked stream for those who are less sick. A screener will greet patients to determine the severity of their condition, and the Centre will care for ambulatory patients who can be seen and discharged quickly. Approximately half of our ED patient volume can be managed through the new rapid assessment space, resulting in faster evaluation and care.
UHN’s Emergency Physicians have launched PHONE CONNECT – an innovative solution to keep vulnerable patients digitally connected to health care providers. Placing digital equity at the centre of care, the program distributes cellphones and SIM cards to vulnerable patients who are under investigation of COVID-19 infection but who lack access to a telephone, need to stay connected to resources, and are unable to reach or be reached by medical professionals. With no access to a phone, it is a challenge for patients to follow up on diagnostic imaging tests, social work consults, virtual care and contact tracing. PHONE CONNECT can change all of this and slow the spread of the virus among the vulnerable.
Want to Learn More?
News & stories
ER doctors gave cell phones to their patients and the results were stunning
The Toronto Star
Toronto ERs feel weight of downtown condo boom
The Toronto Star
Frontline photos ensure “our story is not forgotten”
UHN News
One ER doctor’s photos from the coronavirus frontlines
MacLean’s Magazine 2020
Contact Information
Afsheen Jiwani, MBA, CFRE
Senior Campaign Director, Major Gifts
647-502-7538
[email protected]