In a new study published in Nature Medicine UHN researchers have identified specific DNA changes that can predict a patient’s risk of cancer spreading to the brain, offering new approaches to managing patients and improving health outcomes.
The spread of cancer to the brain, known as brain metastasis, significantly reduces patient survival rates, with a median patient survival of only 10 month to 16 months. Unfortunately, brain metastases are common and make up the majority of brain tumours.
Predicting a patient’s risk of developing a brain metastasis remains a major challenge. Typically, by the time brain metastases are detected, patients are already experiencing headaches or other neurological symptoms, and treatments such as surgery or radiotherapy, are mainly palliative.
There has been an important need for molecular biomarkers of brain metastasis risk to improve outcomes for these patients. However, currently there is no reliable approach to do this used in clinical practice.
“The key here is that our model identifies which patients are at risk of developing brain metastasis early to allow them to be monitored closely and started on treatment as soon as possible,” says Dr. Gelareh Zadeh, co-Director of UHN’s Krembil Brain Institute, Senior Scientist at UHN’s Princess Margaret Cancer Centre, Head of the Division of Neurosurgery at UHN’s Sprott Department of Surgery, and senior author of the study, which was published on Oct. 8, 2024.
A research team led by Dr. Zadeh examined modifications to DNA, specifically DNA methylation alterations, for the new purpose of predicting the risk of developing brain metastases from lung adenocarcinoma (LUAD).
DNA methylation findings have been used for diagnosing and assessing the onset of other cancers, but had not yet been comprehensively evaluated for predicting brain metastases in patients with cancer.
The team developed and validated a computational model to predict patients’ brain metastasis risk based on the DNA methylation signals in their tumour.
‘A really exciting development’
The model determines whether a patient’s risk for developing a brain metastasis within five years of their cancer diagnosis is high or low, and its accuracy was compared to that of traditional cancer stage-based prediction by clinicians.
The team found that their model reliably predicted the development of brain metastases in LUAD patients and was considerably more accurate than the stage-based approach currently used in clinical practice (81 per cent compared to 65 per cent).
“We compiled an extensive DNA methylation dataset of 402 tumour tissue and plasma samples from 346 patients with LUAD, including those who did and did not develop brain metastases, in order to develop and validate our prediction tool,” says Dr. Jeffrey Zuccato, a PhD candidate in Dr. Zadeh’s lab, recent graduate from the Neurosurgery Residency Program at the University of Toronto U of T, Skull-Base Neurosurgery Fellow at the University of Oklahoma Health Sciences Center and lead author of the study.
“Our tool predicts brain metastasis risk more accurately than what has been shown or used to-date, and with an accuracy high enough to ultimately move towards changing our strategies for caring for patients.”
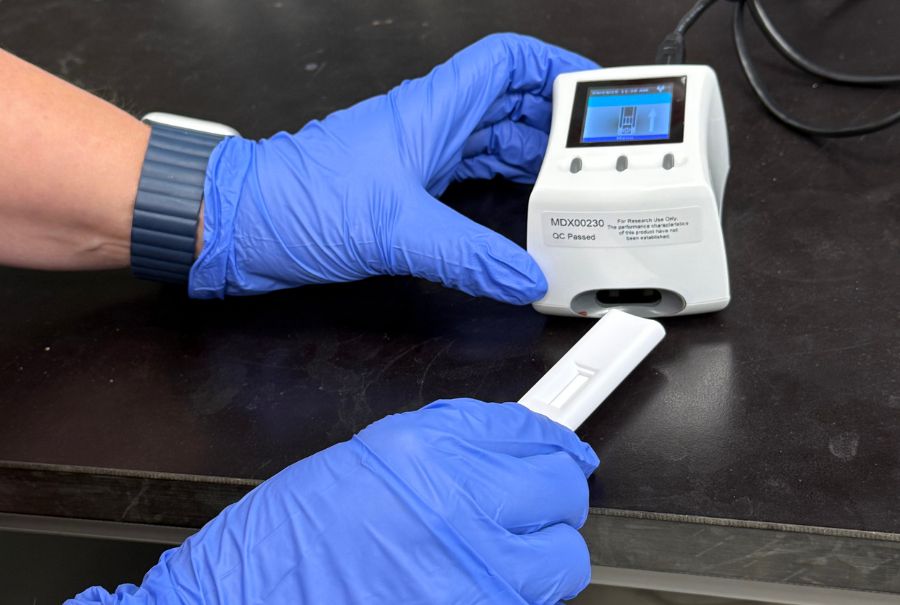
The researchers also identified DNA methylation alterations in patient plasma and built an additional set of models that can be used for reliable liquid biopsy of brain metastases using blood samples, a non-invasive approach.
They are now moving towards translating this work into clinical practice and working on approaches to use these tools in clinical decision-making to improve patient outcomes.
“Understanding an individual patient’s risk has the potential to transform care by enabling us to tailor our management approach to improve patient survival and quality of life,” explains Dr. Zadeh, who is also a professor in the Department of Surgery in the Temerty Faculty of Medicine at U of T.
“This is a really exciting development,” adds Dr. Vikas Patil, scientific associate at UHN’s Princess Margaret Cancer Centre and co-senior author of the study.
“This methylation-based model gives us the opportunity to predict cancer spread and attempt to intervene early to try and prevent it, putting us in a better position to manage this challenging condition.”
This study was supported by generous donors to UHN Foundation among others.