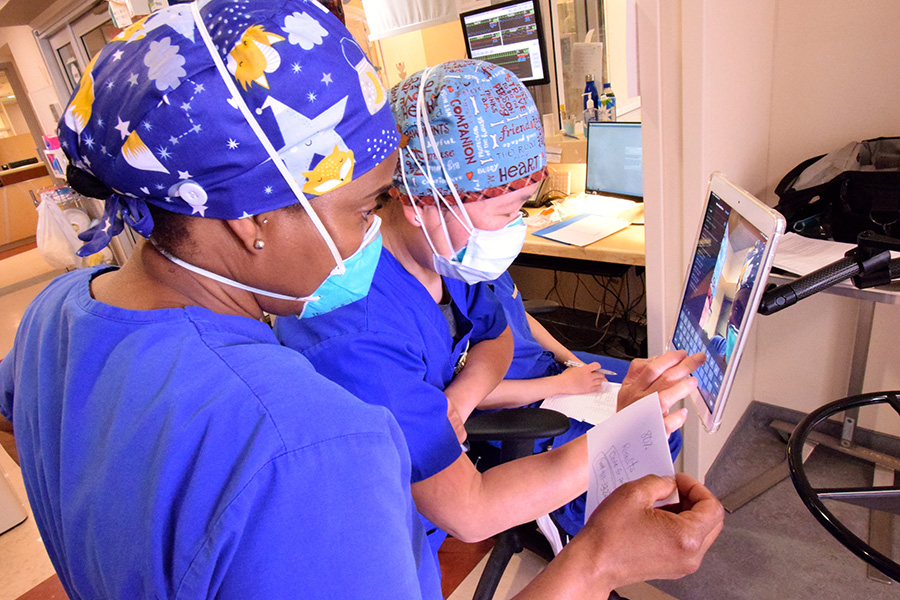
“Nursing works best when you work together, assist each other,” says Karen McFarlane, a registered nurse on the Medical Surgical/Neuroscience Intensive Care Unit at Toronto Western Hospital. (Photo: UHN)
It’s 7:15 a.m. and Karen McFarlane is already putting her new Birkenstock clogs through their paces.
The registered nurse on the Medical Surgical/Neuroscience Intensive Care Unit (MSNICU) at Toronto Western Hospital (TWH) has still not officially begun her 12-hour shift. But today, as she tries to do most mornings, Karen arrived a little early, tucked her lunch into the fridge and relieved her colleague.
“I know how tired you are after working all night,” explains Karen, a nurse on the MSNICU since 2003. In turn, Stacey Williams, who was on overnight, has filled an intravenous (IV) bag with medication for their critically ill patient, saving Karen the task when one on a bedside pump runs out in the next hour.
This is team nursing. Days are long. Stress is high. Little things matter. If you can ease the burden for a colleague, you do. It’s graciousness. It’s camaraderie. It’s how they roll.
“Nursing works best when you work together, assist each other,” Karen says. “It benefits patients, too.”
Briskly making her way across the unit on the second floor Fell Pavilion, Karen offers an upbeat “good morning” to all in her path. She arrives at Pod 105, a narrow strip of four rooms. Each houses a patient on a ventilator. Three have COVID-19, including the woman, in her 50s, Karen will care for today.
This is Karen’s fourth straight day of work, each caring for the same woman. They met about three weeks earlier, when Karen was working a shift on the Critical Care Response Team (CCRT), handling referrals of COVID patients on other floors, aiming to keep them out of the ICU. The patient made progress, determined to continue breathing on her own and avoid connection to a ventilator. But each time, she suffered a setback, finally having a breathing tube inserted and being moved to Pod 105.
“Her lungs are very scarred,” Karen says. “COVID is hard on the body.”
Just after 7:30 a.m., Karen dons personal protective equipment (PPE) for the first of countless times this day. Sanitize hands. N95 mask. Gown. Face shield. Gloves, making sure to pull them over the wrist cuffs of the gown. It’s a precise and vital routine in caring for all COVID-19 patients but particularly this woman – a conventional mechanical ventilator wasn’t working for her, so the respiratory therapists (RTs) switched to a high-frequency oscillatory ventilator (HFOV), which emits an airborne discharge.
Joining Karen is Hye June Chun. June, a registered nurse (RN) with about 10 years of experience, is taking a 10-week course through the Michener Institute of Education at UHN to become an ICU nurse. This is one of 18 clinical shifts in the program and Karen is her preceptor, supervising her for the day.
Fully clad in PPE and having checked each other to make sure there are no gaps in protection, Karen and June push open the door to enter the room and conduct a thorough assessment of the patient to begin their shift. The woman in the bed, who is paralyzed and sedated with a breathing tube in her mouth, has made progress. Slowly. For two days, she required 100 per cent oxygen. When Karen and June left 12 hours earlier, she was at 90 per cent. Overnight, the RT was able to lower it to 70 per cent.
“You’re heading in the right direction, my dear,” Karen tells the patient. “Keep it up.”
Karen’s tone is warm, upbeat, the way you imagine a hug might sound. It’s also just a few decibels shy of a shout. Unlike a conventional mechanical ventilator with its deeper and quieter breathing rhythm, the HFOV is shallower, faster and much louder, reminiscent of a train chugging down the tracks.
For the next hour, Karen and June do a complete, head-to-toe assessment of the patient. They start by examining her eyes with a flashlight to ensure they dilate, indicating neurological function continues despite sedation and paralysis. Each of eight IV lines, which carry a different medication from a pump to the patient, are checked for leaks and to make sure that it’s the right medication and the right dose being infused. The nurses reposition her in the bed, brush her teeth, swab her mouth, apply lip balm. They raise a curtain around the bed before washing the woman’s face and the rest of her body. The entire time, they talk to her, explaining what they’re doing.

Dignity. Respect. Privacy. Those can be in short supply for people who are critically ill with COVID-19. That’s why it’s so important to Karen that she show the patients she cares for that they are loved.
“Nobody asked to be here. Nobody wants to be here. But people get sick,” she says. “I nurse everybody as if it was my family member in the bed, or me in the bed. I ask, ‘what would I want?’
“Even though she’s not responding, I still tell her what we’re doing. I still know that I should close the curtains. Dignity is very important when someone is not doing well, or you know they’re going to die.
“You want to make sure that to the very end the person has their dignity intact. I’m very passionate about that.”
It’s a passion which has deepened due to Karen’s personal experiences.
Karen’s mom died in January 2019 after a 12-year battle with cancer. Last November, her dad was hospitalized with COVID-19. Six months later, he’s not fully recovered but is off oxygen, walking regularly and recently returned to his home, where “he’s cooking up a storm,” she says.
“My mom taught me what it was like to lose someone so close,” Karen says. “And, through my dad, I learned how hard it is for families to not be able to be here to visit their loved ones in a time of need.
“So, you’re trying to console people but you’re crying, too. It’s human, but it’s still a horrible feeling. It’s that your heart is involved. You can’t help that. You feel for people and know what loss is like yourself.
“A few months ago, I had a lovely patient die. I cried like it was my mom.”

The morning assessment complete, Karen and June remove and dispose of their gowns and gloves in bins inside the room. They emerge, remove their face shields and sanitize their hands. It’s the same meticulous process each time, whether they’re in the room for an hour or a just minute.
Once outside the room, the nurses chart all their observations and procedures conducted when inside. It’s information filled out each time they emerge from the room, some on paper, others electronically. It’s a process repeated after each interaction with the patient. And today, it’s June’s job to handle it.
“How are you doing with the charting?” Karen asks about 30 minutes later.
“I think I’ve done it,” June replies.
“You think, or you know? I want to hear confidence,” Karen says enthusiastically. They both laugh.
During a rare break in the morning routine, the four nurses of Pod 105 take a seat. The other three admire Karen’s new clogs, which her sister recently sent from Maryland. Soft insoles for comfort during a 12-hour shift, removable and easy to wipe clean, they get high marks from the discerning audience.
“I wanted some army green shoes because I’m ready to fight COVID-19,” Karen says with a chuckle.
What’s clear throughout the day, is how many weapons and people are involved in that battle. During rounds at about noon, a lead physician, resident and pharmacist are among those discussing the care plan for each patient. In a span of just a few hours, Karen and June’s patient also undergoes dialysis, gets an X-ray, has a couple of RTs adjust the HFOV, and a physician and RT repair a wound on her neck caused by the vascular catheter which is delivering medication into her body. Each of them are supported by teams cleaning, supplying fresh gowns, masks and gloves, and moving equipment.
“It’s a multi-disciplinary team looking after every patient,” Karen says. “It’s not one individual.”
Shortly after 4 p.m., Karen makes a phone call to the patient’s family. She keeps it high level, stays clear of medical terms and tells them their loved one is still critically ill, paralyzed and sedated. She recounts the change in oxygen over the past 24 hours.
“The oxygen is coming down,” Karen says into the phone. “It’s not great, but it’s better than it was.”
A few minutes later, Karen is back in PPE and at the bedside. With an iPad affixed to an IV pole, she’s connected the family to their loved one via FaceTime. They talk to the woman, sing, pray.
“Thank you so much,” one of the family members says to Karen as the call ends after 10 minutes.
“You’re so welcome. We’re taking good care of her.”
Karen has facilitated many of these calls. They’re never easy but she knows they’re vital.
“Even if they can’t have a conversation with them, at least they can get a visual,” she says. “It’s hard because they know their loved one is not doing well, they know they’re really sick.
“But laying eyes on them can offer some comfort.”

At 6:30 p.m., Karen is back into the room for one final time on her shift. June has left for a meeting with fellow ICU trainees elsewhere on the unit, so Karen is by herself as she again repositions the patient – once every two hours all day to avoid pressure ulcers – and checks the reading on each of the medication pumps beside the bed to help her calculate how much has been used over the past 12 hours.
After emerging from the room, Karen charts everything she did. She then turns her attention to filling an IV bag of medication for Stacey Williams, who will soon arrive for the night shift.
“She did it for me this morning, so I’m just paying it forward,” Karen says.
When Stacey arrives, Karen takes her through in detail what she describes as “a tough day” for the patient. There is talk of the woman’s oxygen levels, medication changes, neurological responses and heart rate. The charting – paper and electronic – is reviewed. Karen discusses the FaceTime call.
“They know the magnitude of how ill she is,” Karen says of the patient’s family.
Then, Karen is on her way. After 12 hours, there’s certainly less bounce in her step. But she remains resolute in her positive outlook and proud of the work she and her colleagues do everyday.
“As devastating as this disease is, with all the lives lost and families left distraught, I truly believe we can do good things during this horrible time,” she says. “We can be a ray of light for people.”


