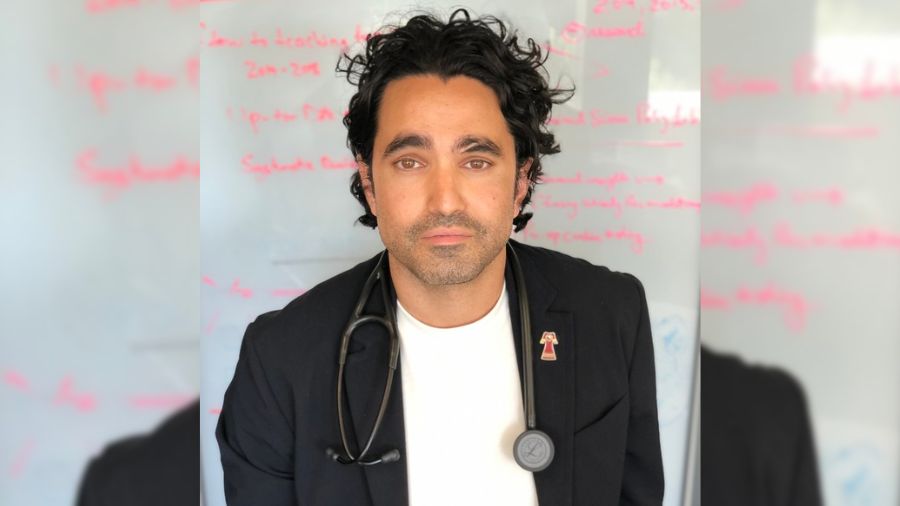
UHN social workers, (L to R), Amy McLean, Nicole Furey and Lindsay Bailey, support, comfort and advocate for patients in the Emergency Department at the Toronto General Hospital. (Photo: UHN)
It’s 9 a.m. and Nicole Furey has unfinished business.
A social worker in the Emergency Department (ED) at Toronto General Hospital (TGH), she begins the day’s shift the same way yesterday’s ended – trying to help an elderly patient keep safe. The man, in his 70s, came to the ED by ambulance the previous afternoon following a fall at home, where he lives alone.
Recovered from COVID-19 and with several comorbidities, Nicole fears a repeat if he’s sent home.
It’s a familiar and disturbing pattern during the pandemic for the two most common types of patients referred to the social work team in the ED – seniors not coping well at home, and people with addictions, and very often mental health challenges, who are also experiencing homelessness.
“People’s social lives and their social networks have changed through the pandemic, and they’ve shrunk,” says Nicole, a social worker at UHN for the past five years. “For people who were already isolated, that can be the difference between managing in the community and coming to the hospital.”
That’s the scenario on this morning for Nicole and her colleague, Amy McLean, who is redeployed from Toronto Rehab, Lyndhurst Centre, where she’s an outpatient social worker in spinal cord rehab.
In addition to the senior, who they hope to get into rehab for a few weeks to gain more independence, the ED team has also referred to them two men who came in overnight, after evening shift social worker Lindsay Bailey had left for the night. Both men are experiencing homelessness and have addictions.
One of them is asleep on a stretcher near the Nursing Station. Amy goes to talk to the other one, who has just woken up. She offers to help him find a shelter bed, maybe as a path to more community support. He refuses. And, after finishing some juice and a sandwich Amy provided, he’s out the door.
“I can’t make somebody want help,” says Amy, a social worker at St. Joseph’s Health Centre in the west end of Toronto from 2002 to 2009, including in the ED, before rejoining the workforce last October when she started at Lyndhurst. “But I can treat them with kindness and respect as I offer it to them.
“You have to respect the autonomy of people.”
Amy, who volunteered for redeployment, is asked what it’s like being back in the ED.
“Sad to say, it does feel a little like riding a bike,” she says with a laugh.
Emergency medicine is often a sprint. Patients are rushed in, triaged and treated. Social work in the ED is more of a marathon. It’s about connecting patients with the right community resources, offering a compassionate ear to someone terminally ill or a sandwich to an individual living on the streets.
“Advocacy is a huge part of what we do,” says Lindsay, who has worked at UHN for the past year.
“More isolation, less access to resources, especially in-person resources, is one of the glaring challenges the pandemic has brought on. It just makes it that much tougher for people to get the help they need.”
UHN has more than 150 social workers who practice across all medical programs. The many roles they play include helping patients, families and caregivers access and navigate the appropriate care, cope with the impact of an illness or hospitalization from an emotional, financial and practical perspective, ensure patient wishes and needs are heard, provide counselling and support, and help access community resources.

During the pandemic, social workers in Intensive Care Units (ICUs), COVID wards and EDs, have also worked with other members of the care team to comfort critically ill and dying patients, connect them virtually with family, and also offer grief counselling and support for loved ones of those who pass away.
Nicole worked upstairs in the ICU during the first wave of the pandemic. It was difficult. She talked to and played music for patients who were intubated. And, when someone died, she would follow up with the family to offer comfort and practical knowledge about claiming a body or planning a funeral.
“Most people have never done that before, so you try to put yourself in their shoes and be as compassionate as you can,” Nicole says. “Nothing can prepare you for it, but at the same time, unfortunately, we’ve done this so many times that we know what people need at a time like that.
“And really, you just try to be kind. There’s a shortage of kindness in the world right now.”
Shortly after noon, an elderly patient with COVID-19 is rushed into an ED bay. The Code Delta Team, all clad in personal protective equipment (PPE), begins the process of inserting a breathing tube. From the moment the intubation procedure begins, it’s clear this is an all-too-common occurrence here. All but those involved go about their business.
Once the procedure is complete, Nicole checks in with the ED physician, who confirms that the patient’s family is aware that the intubation happened, so she does not need to contact them. She makes a mental note to pass on that information to her social work colleague in the ICU. Minutes later, the patient is on the way there.

A short time later, it’s Nicole’s turn to don the PPE. She’s trying to wake the young man on the stretcher, who has been having an increasingly fitful sleep and crying out. She repeatedly uses his first name. Softly. Then, a little louder. He stirs but keeps dosing. She persists. He engages, agreeing to let her get him something to eat. Seeing his dirt-caked bare feet, tattered clothes and filthy hands, she also convinces him to take new shoes, socks and pants.
Nicole and Amy go through donated clothes and shoes in a pair of lockers looking for his size. They also grab a “hygiene kit,” which includes socks, underwear, toothpaste and a toothbrush, a comb, soap and other toiletries.
“At the bare minimum, we try to send people out with some basic dignity,” Nicole says. “If all he takes today is juice, a sandwich and some shoes, that’s okay. Maybe next time he’ll open up about what he needs from us because he knows we’re a safe place to come.
“For some people, it’s literally taken years to help them.”
It won’t happen on this day. Not with this young man. He drinks some juice and eats a couple of sandwiches, but after putting on the gifted pants, socks and shoes, he’s gone. The hygiene kit lies on the stretcher.
Nicole is quick to shake her head when asked if she feels defeated when someone leaves without taking any more than just basic help: “Honestly, if I did, I would feel defeated too often,” she says.
Social work here is about the team. As new referrals come in, the person most available steps up to take it. On more complex cases, or those that take longer to resolve, all three of them will be involved, working together and with other Allied Health professionals, to best support the patient’s needs.

Across the ED, Amy is meeting with a cancer patient who is terminally ill. The woman came in for pain but was referred to the social work team because she was crying and appeared to need to talk.
“She was just looking for an empathetic ear,” Amy says later, after a long chat with the woman, getting her some answers from the ED pharmacist on medication side effects and referring her to Spiritual Care.
“You’re human. It feels good when someone wants to talk to you and happily accepts what you’re offering and feels there’s benefit to it.”
At 2 p.m., Lindsay arrives to start her shift. The three social workers huddle up to recap the day so far.
There’s success to report on the senior who arrived nearly 24 hours earlier. After several rounds of paperwork, phone calls to his family and rehab centre where he went after his bout of COVID-19 and consultations with ED colleagues about wound care and his medications, he’s going to transfer.
Before dinner, he will be off to rehab.
“All we wanted was to try and help him regain some of his functional independence and quality of life,” Nicole says. “So, in my mind, we got him to the appropriate level of care, and that’s a success.”