Dr. Michael Randazzo is a UHN General Internal Medicine (GIM) Clinical Associate treating COVID-19 patients. (Photo: UHN)
It’s the start of his ninth shift in a row, and yet Dr. Michael Randazzo is bounding up stairs in a cavernous Toronto General Hospital (TGH) stairwell. He can’t wait to get to his first patient.
“The fire still burns,” says the General Internal Medicine (GIM) Clinical Associate just two years removed from his fellowship. “We’re going to go until there is no more need for it.”
Perhaps that’s youthful exuberance, but over a year into the brutal COVID-19 pandemic Dr. Randazzo’s unwavering determination is an outlook many of us could use a dose of these days.
By 7:50 a.m., he’s sitting in a small open office area off the 6 Eaton South COVID ward Nursing Station getting briefed by Dr. Rymon Rofaiel, the overnight physician, or “nocturnist” on the status of 13 COVID-19 patients. Several are in worse condition and needed more help with supplemental oxygen as the night wore on.
Oxygen levels are a litmus test for severe COVID-19 patients and their recovery. Here’s why. The coronavirus is a respiratory disease that in acute cases infects the lungs. They fill with fluid, mucous and other debris, and can progress to pneumonia. This makes it harder to breathe, and harder for the lungs to do their job of removing carbon dioxide from the bloodstream and infusing it with oxygen. Thus the need for supplemental oxygen.
The more oxygen needed – the worse the condition.
At 8 a.m., Dr. Randazzo is on the move again, down the stairwell to team up with nurse practitioner (NP) Sheila Lingan, who is waiting for him on 5A Eaton, another TGH COVID ward. She is equipped with a workstation on wheels – the mobile medical cart with computer and instant access to patient records.
For the next few hours, the two will assess patients on the two TGH COVID wards and generate a treatment plan for the day. At the same time, another doctor/NP pairing takes care of the other half of the COVID patients on 6 Eaton South and 5A.
It’s a marvel to think none of this existed back in March 2020. When coronavirus cases started showing up at UHN Emergency Departments (ED) there were no COVID wards to treat the up to 15 per cent of patients suffering from severe symptoms and needing to be admitted.
This was unknown territory. The challenge was threefold. These patients can’t stay in the ED, and they are not sick enough for the Intensive Care Unit (ICU). So where do you put the severe cases without risking spread of the virus? Who’s going to treat them? And what are the treatments, if any?
These medical conundrums fell to GIM, the Swiss Army knife of internal medicine. GIM specialists are trained in complex care. Skilled at handling patients with multiple conditions, comorbidities, both acute and chronic illness, as well as trained in geriatric care.
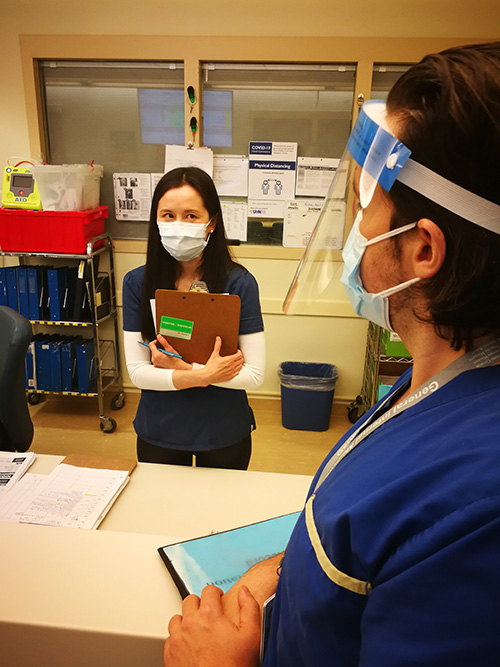
“We’re super comfortable with uncertainty,” explains Dr. Jessica Liu, the GIM Site Lead at TGH. “With COVID, we had to become experts in something no one’s an expert in. We read case reports from Wuhan. We put together protocols. We looked at what Harvard and Yale and all those places were doing. We developed a handbook… and setup this rounding system based on what a resident in Spain was doing.”
Literally overnight, the GIM wards at Toronto Western Hospital and TGH expanded their complement of 200 beds to accommodate treatment of up to 60 COVID patients. And in the beginning, fear of what could happen to staff was palpable.
“People were scared. We did our wills. I left a list of all my passwords with my husband… you’re so terrified… then you actually get in a room with a patient. And it’s just a regular person who needs help,” says Dr. Liu, who adds that the GIM mantra became one of “pitching in and contributing.”
To underscore that mantra, both Dr. Randazzo and Ms. Lingan volunteered for their tour of duty on the GIM COVID ward. Today, Dr. Randazzo is winding up his fourth stint of day shifts, in addition to numerous “nocturnist” shifts. Several weeks ago Ms. Lingan was a cardiovascular surgery nurse at the Peter Munk Cardiac Centre. With surgeries ramping down during the third wave she was inspired to pitch in and help her frontline colleagues. Plus, there was a personal motivation.
“I actually have a family member who tested positive in wave one and it was a terrible situation for her… so I volunteered.” says Ms. Lingan.
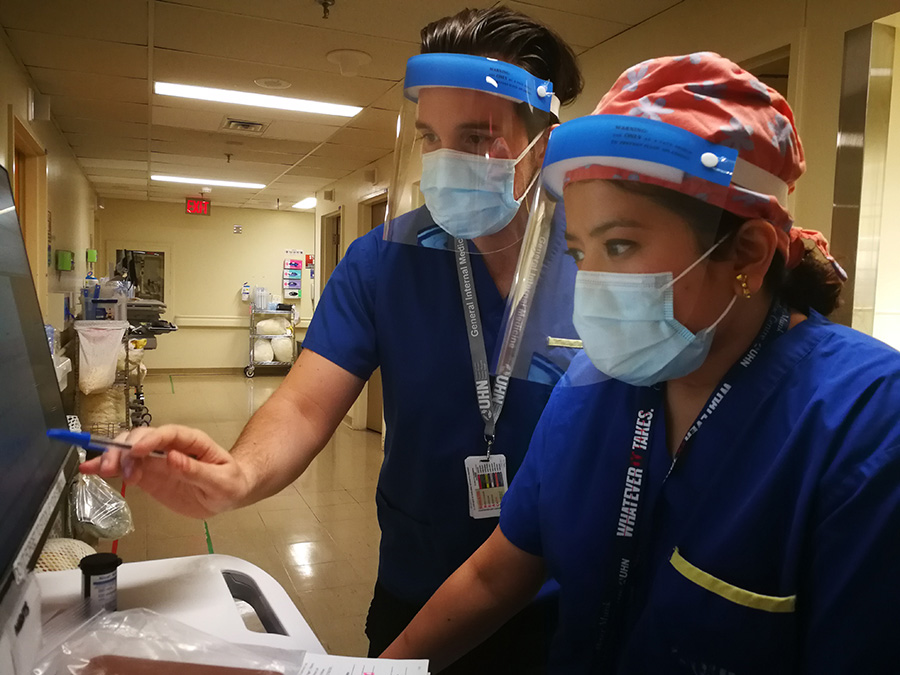
The team of Dr. Randazzo and Ms. Lingan work with calm, systematic precision as they methodically make their rounds of the ward. They are in sync, as if they have been doing this for years.
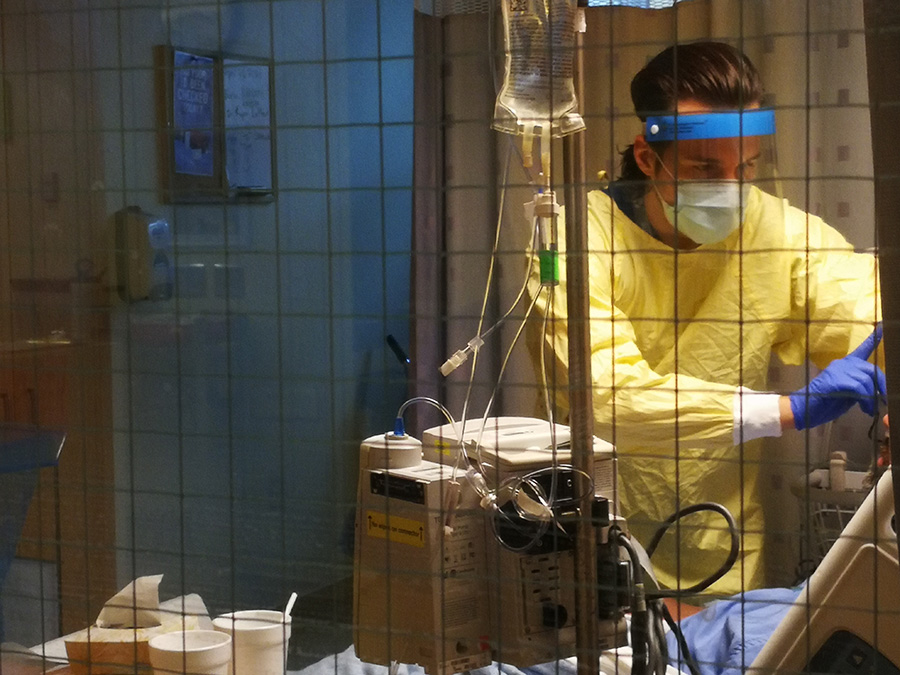
They wheel up to the entrance of each room. Dr. Randazzo carefully dons personal protective equipment (PPE). It’s quiet in the hallway, except for the rising hissing sound of the life-sustaining oxygen machine as he enters each room.
After the patient is examined, Dr. Randazzo sheds his PPE at the doorway inside and exits to discuss the patient plan with Ms Lingan, who enters every notation and action into the electronic patient record (EPR).
One patient, a 40-year-old male, has been here a few days. He has shortness of breath, decreased appetite, is weak and dizzy, and overnight his need for oxygen increased. The COVID infection has not yet peaked.
Most patients in the GIM COVID wards will recover. The average stay is five days to a week, some up to two weeks. About 10 per cent will worsen and go up to ICU for ventilation.
Ms. Lingan says the one thing all patients have in common is fear.
“One thing I get asked a lot is if they’re going to make it, that is the first question… so they’re pretty scared,” she says. “I just say you’ve got to stay positive, stay in touch with your family, and we are caring for you.
“Honestly, I don’t know if that helps, but that’s the only thing I can say as I don’t want to give them false reassurance.”
Dr. Randazzo and Ms. Lingan arrive outside the room of a patient in his 30s, a spouse and two children at home. The patient is stable, on just one litre of low-flow oxygen and nearing discharge. All that’s left is the “walk test” – a lap around the ward unaided, and breathing on their own. Then, the patient’s blood oxygen level is measured. This is how saturated the bloodstream is with oxygen. A score of 92 per cent or higher is needed to go home. If all goes well –hopefully tomorrow.
Next up, the precarious case of a 60-year-old patient on high-flow nasal oxygen, or HFNO. That’s the highest level of three oxygen supplement options, after low-flow nasal clips and the TAVISH mask have been exhausted. HFNO is where oxygen is literally being pumped in to the body. In this patient’s case, it’s doing about 90 per cent of the work of providing oxygen to the bloodstream. ICU staff are alerted.
In addition to oxygen supplement, Dr. Randazzo and the GIM team have a few medications at their disposal to treat some of the COVID symptoms. There’s dexamethasone, a steroid that reduces the amount of inflammation in the lungs caused by the viral pneumonia. Remdesevir, an antiviral, is also available, although Dr. Randazzo says there’s not a lot of evidence it reduces mortality. And there’s Tocilizumab, another anti-inflammatory typically used to treat rheumatoid arthritis, but now in short supply in Canada.
At 9:05 a.m., Dr. Randazzo breaks from his rounds for an Allied Health update via phone to discuss all the 5A and 6S COVID patients. The team of social workers, physiotherapists, occupational therapists, charges nurses, and transitional care coordinators take care of everything from patient psychological needs to ensuring a smooth discharge from care.
Dr. Randazzo flags to the Transitional Care Coordinator that one of his patients is being discharged today and needs at-home assistance, but is refusing. In turn, he is warned about a patient admitted overnight who is on “constant observer” status after taking a swing at a nurse.
On his way back to rounds, Dr. Randazzo sees the Critical Care Response Team, which helps with the management of more challenging cases in the ED, ICU and on COVID wards. In their discussion, it’s recommended one of the worsening patients be “proned” – turned on their stomach for up to 16 hours to help distribute breathing more evenly and protect the lungs.
For a physician just starting his career, this pandemic has been a crash course not only in mastering effective COVID-19 treatments, but managing emotions.
“You’re a physician, you’re trained to manage people and all those kind of things but… there’s always that human side,” explains Dr. Randazzo. “It’s been difficult to see and it has had a lot of impact on us.
“You try not to take it home right? Some days it’s harder than others.”
Dr. Randazzo and Ms Lingan travel up to the 13th floor of the Eaton building to check on one more patient who has made a full recovery from COVID. All that’s left is a walk test.
A pulse oximeter clip to measure blood oxygen level is put on the patient’s left index finger. The reading must be 92 per cent or higher for the patient to be able to go home.
The walk begins. The steps are slow, steady. Dr. Randazzo is at the patient’s side, murmuring words of encouragement. They round the last corner and are outside the patient’s room where Ms. Lingan waits.
Dr. Randazzo presses the oximeter for a readout. The three stand motionless. Waiting for the number. Silence. Then – 95 per cent. The patient can go home.
“It’s the best feeling ever, and so gratifying that the therapy you put them on worked,” explains Ms. Lingan. “He beat COVID.”
“I was really happy for him,” adds Dr. Randazzo. “When you see someone who was really sick a week ago, it’s nice to say I did my part in helping.”
If there are silver linings in this pandemic for Dr. Michael Randazzo, it’s these moments of victory. And the knowledge that in this unrelenting battle he’s part of an amazing team.
“I love it here because of the people,” says Dr. Randazzo, “You know when you go through something like this, it makes you say this is my home.”