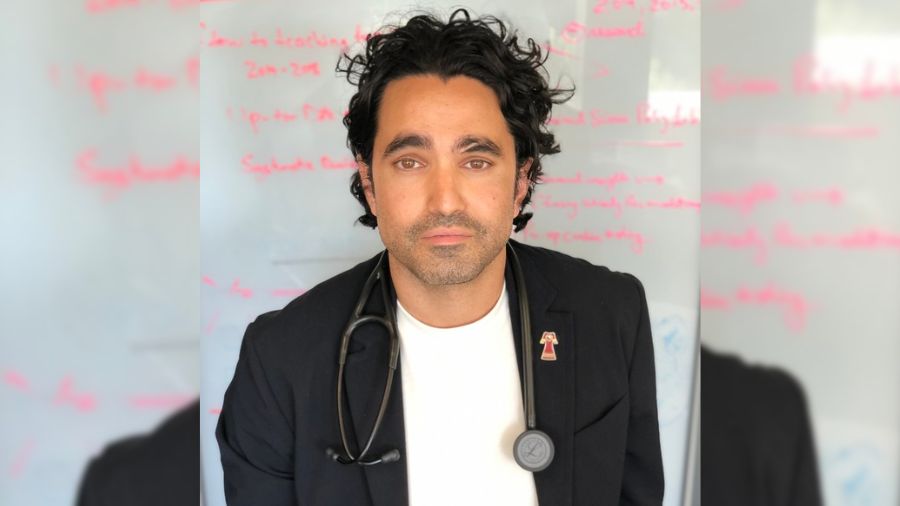
Renz Madriaga, support clerk with UHN’s Connected Care Clinical Hub, says, “knowing our team makes a difference in people’s lives each time I go to work is motivating.” (Photo: UHN)
Suddenly unemployed from his restaurant job at the outset of the pandemic, Renz Madriaga was looking for work. But he didn’t just want a job. He wanted to make a difference. He wanted to give back.
Aware of how overwhelmed the healthcare system was, Renz sought a job in the field. He joined University Health Network’s Connected Care Clinical Hub in a support role, working with various communities within the Mid-West Toronto Ontario Health Team.
“Knowing our team makes a difference in people’s lives each time I go to work is motivating,” says Renz, who now alternates between COVID-19 assessment centres and vaccination clinics.
“I love doing this, it feels rewarding to be a part of it and serve the community.”
The UHN Connected Care team’s rapid deployment of the Clinical Hub early in the pandemic was a critical enabler to the UHN’s broader integrated care strategy, bringing together dozens of multi-disciplinary members of TeamUHN to support patients with coronavirus at home.
UHN’s Connected Care team works alongside members of the community to provide equitable and timely access to care. The hub’s dynamic growth has enabled virtual and in-person care, community initiatives and helped streamline social supports.
Dr. Chris Chan, Medical Lead for UHN Connected Care, says many types of care can be delivered outside the walls of a hospital, allowing patients to avoid going to the Emergency Department (ED) or being admitted to hospitals with COVID-19, pneumonia or influenza-related complications.
“In the past we have struggled to find ways to organize so that patients and care providers feel confident that individuals can be well supported at home,” says Dr. Chan. “With the Clinical Hub model, we are doing that.”
Since April 2020, an immeasurable number of ED visits and readmissions have been prevented in partnership with programs such as the UHN Connected Care Clinical Hub. To date, the Clinical Hub has had 53,000 visits and more than 30,000 referrals.

Health Equity
The UHN Clinical Hub is effective at reaching the city’s most vulnerable and immunocompromised patients by acting as a central care and coordination point. It continues to play a critical role in Toronto’s broader pandemic response and meet the ongoing health care needs of diverse communities.
Determined to bridge systemic barriers to health care, the UHN Connected Care team deploys staff to shelters, community centres, gymnasiums and residences in neighbourhoods hit hard by COVID-19 to ensure community members get the care they need.
“Health equity has been a defining issue of this pandemic and we are determined to use the advancements we have made to get Torontonians the care they need,” says Shiran Isaacksz, Vice President, UHN Connected Care. “The incredible ambassadors, leaders and care providers in the community know their residents the best.
“Connected Care has been fortunate to support their efforts through strong and collaborative partnerships, ensuring a community-led approach.”
Throughout his work with the UHN Clinical Hub, Renz helps community members feel more at ease as they interact with the health care system, whether that’s in COVID-19 assessment centres or vaccine clinics. Renz also supports communities by doing door-to-door campaigns to sign-up people who might need the vaccines brought to their neighbourhoods.
“I just think about how I would want to be treated and I do the same,” he says.
“Being able to communicate in multiple languages is core to what we do. We do our best to have volunteer translators but if no one is around, we have our good friend Google translator to do the job.”
Accessibility
Accessibility to care continues to be a barrier in community support. Virtual care initiatives allow for improved patient outcomes, reduced patient volumes, and are at the forefront in assisting with many lingering psychosocial challenges which have been exacerbated by the pandemic.
Patients referred to the UHN Connected Care Clinical Hub are seen within 24 hours, which is especially critical for assessing treatment options for people with COVID-19.
“Delivering an excellent patient experience is always at the core of what we do,” says Katey Peirson, a nurse practitioner with UHN’s Connected Care Clinical Hub. “We give them treatment options and make sure they’re improving.
“We strive to keep them out of hospital, and this includes access to priority testing and therapeutics.
“The virtual work really blossomed during the pandemic and I think its something that is here to stay,” says Katey “Nobody in the community expects to get regular calls as follow-up – it’s unheard of, but it is critical to a patient’s ability to self-manage and continue the recovery process.”
New Models of Care
The quick pivot to support UHN’s surrounding communities – and help reduce the strain on health human resources – meant taking innovative approaches such as hiring team members with valuable transferable skills gained from outside the health care sector.
Renz Madriaga was one of them.
“In the service industry you learn how to speak to people and really read the room on what kind of mood they’re in and what they might need,” says Renz. “Many people are already sick and not feeling great, I try to treat them really well and hope to make their experience better.”
The addition of fresh perspectives is contributing to a new era of community health delivery.
“The key is to be able to work with our colleagues across the continuum to effectively manage patients at home, but also provide timely access to acute care when needed,” Dr. Chan says. “We have that opportunity here with this Clinical Hub and we have the partnerships to expand and make this work as a key tool for all integrated models of care.”
Katey adds: “COVID is a big piece of what we do now, but it’s a small piece ultimately of what this program will continue to evolve into. The possibilities are endless and I’m happy and thankful to be along for the ride to see how things continue to grow.”