A new study published in medical journal The Lancet and presented at the International Stroke Conference in Los Angeles, shows strong promise for efficacy of a drug that could reduce stroke damage. Nerinetide (NA-1) is the first neuroprotective therapeutic agent in the world to demonstrate improvement in the outcomes of patients with acute stroke, which occurs when there is a blockage in an artery that supplies blood to the brain.
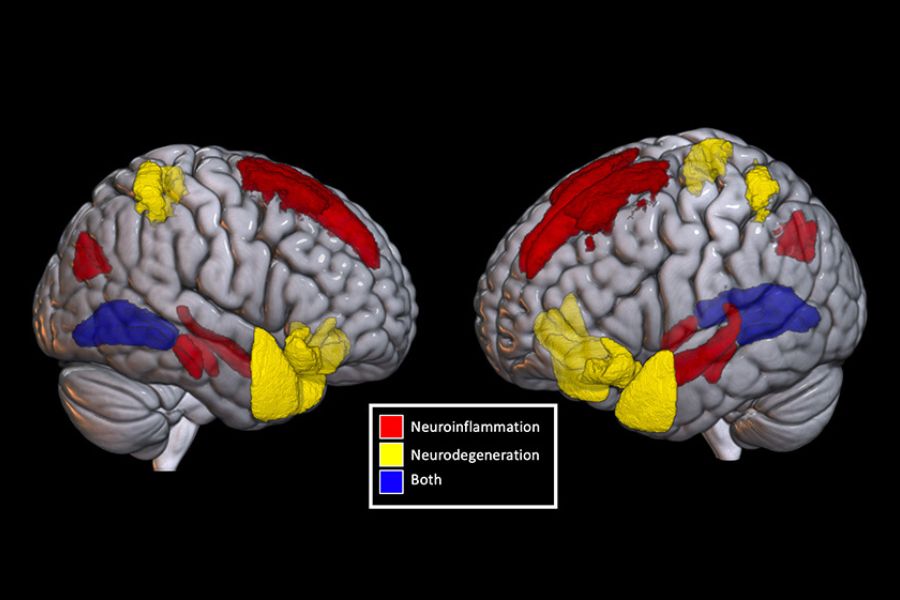
During a stroke, the brain loses 1.3 million neurons per minute. Nerinetide enhances the resilience of brain cells to withstand the lack of blood supply during a stroke, therefore reducing its damage. It was developed by Dr. Michael Tymianski, a neurosurgeon within the Sprott Department of Surgery and Senior Scientist with the Krembil Brain Institute at Toronto Western Hospital.
“This is a terrific example of the importance of investments in fundamental research and how they fuel the development of new therapies that can impact the patients we serve,” says Dr. Brad Wouters, Executive Vice President, Science and Research at UHN. “Dr. Tymianski and his team are motivated by the unmet needs of our patients and they are creating change through discoveries in basic research.”
“Therapeutics in stroke is an area that has been a wasteland for decades and I think today’s announcement represents a step in the right direction,” says Dr. Donald Weaver, co-director of the Krembil Brain Institute. “It demonstrates that drugs that can meaningfully treat people with stroke are possible, and this research shows us the route to how to get there.”
This work is the result of more than two decades of scientific research by Dr. Michael Tymianski and his research and development team, which first began at UHN in Toronto and continued under NoNO Inc., a biotechnology company founded by Dr. Tymianski.
There have been many milestones along the way, including the discovery of a protein called PSD95, which can impact the severity of stroke damage and the identification of a molecule (the first iteration of nerinetide), which is able to block the protein in preclinical models.
This study is the result of a Phase III clinical trial called ESCAPE-NA-1, involving more than 1,100 stroke patients worldwide. Nerinetide was administered to patients selected for endovascular thrombectomy, a procedure in which a tube is inserted through an artery in a patient’s groin, then, using imaging, is guided to the brain, where a retrievable stent removes the clot.
The study found that implementation of nerinetide, without prior administration of alteplase (also known as tPA), improved functional outcome, reduced mortality and decreased infarct volume (a measure of the extent of brain injury) among acute ischemic stroke patients.
The trial was led by Dr. Michael Hill, a neurology professor and director of the Calgary Stroke Program, and Dr. Mayank Goyal, a professor of radiology at the University of Calgary. It is the largest trial involving endovascular thrombectomy in history and the largest ongoing acute stroke trial globally.
“It takes many years and the talents of countless individuals to take an idea, a concept, and to translate that to a drug,” says Dr. Weaver. Dr. Tymianski has been working on this approach to stroke for two decades.
“I think that a lot of people would have given up. He did not. Kudos to him for having the persistence and the diligence to continue with this idea and kudos to UHN for fostering an environment where research like this is possible.”
[su_heading size=”18″]The path to the clinical development of nerinetide (NA-1)[/su_heading]
- 1990s – As a Senior Scientist with the Toronto Western Research Institute (now the Krembil Research Institute), Dr. Michael Tymianski’s research focuses on why brain cells die when they are deprived of oxygen and glucose.
- 1999 – Dr. Tymianski’s lab discovers that a protein in brain neurons called PSD95 is important in mediating stroke damage. The team turns its attention to determining how to block this protein to reduce the brain’s vulnerability to stroke damage from an ischemic Results are published in Science.
- 2002 – The research team reports that a molecule developed in their lab, the first iteration of the eventual drug nerinetide, blocks PSD95 protein and reduces stroke damage in preclinical models. Results are published in Science.
- 2003 – Dr. Tymianski founds NoNO Inc., a biotechnology startup company aimed at further developing this class of therapeutic molecules called “PSD95 ”
- 2005 – 2012 – The team continues its research on PSD95 inhibitors, publishes several papers on their properties and mechanisms of action. Multiple labs around the world independently confirm the results published by Tymianski’s team and extend their findings to other diseases including epilepsy, traumatic brain injury, Huntington’s disease and Alzheimer’s disease.
- 2012 – The team publishes a paper showing that nerinetide can reduce the damaging effects of strokes in primates, using experimental approaches that simulate the strokes incurred by patients who undergo endovascular surgery for aneurysm repair. The study is published in Science Translational Medicine.
- 2012 – The team publishes a multi-centre, randomized, placebo-controlled trial in 185 patients showing that nerinetide reduces stroke burden in patients who undergo endovascular surgery for brain aneurysm repair. This world-first – showing that neuroprotectants can reduce stroke damage in humans – is published in The Lancet Neurology.
- 2012 – The team publishes further research in old-world primates which bear genetic, anatomic and behavioural similarities to This time, the research shows how a “PSD95 inhibitor” prevents brain cell death and preserves brain function when administered after a major stroke has occurred. The study’s experimental approaches simulate protocols that are planned for clinical trials in acute ischemic stroke. These protocols include giving nerinetide within the first hour after stroke, and another where nerinetide is given in scenarios that approximate those observed in stroke patients who undergo endovascular thrombectomy. Results are published in Nature.
- 2015 – Launch of a Phase III, multi-centre, randomized, placebo-controlled clinical trial in 558 patients in eastern Ontario and western British Columbia, called FRONTIER. Paramedics in the field administer nerinetide or placebo to eligible stroke The drug is being given approximately one hour after stroke onset, simulating one of the experimental approaches previously tested in primates. The trial is ongoing.
- 2017 – Launch of a Phase III, multi-centre, randomized, placebo-controlled clinical trial in 1,105 patients in Canada, the United States, Europe, South Korea and Australia, called ESCAPE-NA-1. Nerinetide is administered to patients selected for endovascular thrombectomy, simulating one of the experimental approaches previously tested by the team in primates. The trial is led by Michael Hill, a neurology professor and director of the Calgary Stroke Program, and Dr. Mayank Goyal, a professor of radiology at the University of Calgary. It is the largest trial involving endovascular thrombectomy in history and the largest ongoing acute stroke trial globally.
- 2020 – Results of the Phase III ESCAPE-NA-1 are published in The Lancet and presented at the 2020 International Stroke Conference on February 20, 2020