At UHN’s McEwen Stem Cell Institute and Ajmera Transplant Centre, clinicians and researchers are working on the next big development that could cure diabetes and render insulin obsolete – stem cell therapy.
Since its discovery 100 years ago by Banting and Best at the University of Toronto and its first clinical use at UHN’s Toronto General Hospital, insulin has saved the lives of countless individuals living with diabetes.
In a conversation with the Toronto General & Western Hospital Foundation, Dr. Trevor Reichman, Director of the Pancreas and Islet Transplant Program at the Ajmera Transplant Centre and Dr. Cristina Nostro, Senior Scientist at the McEwen Stem Cell Institute discussed their goals to bring stem cell therapies to people living with type 1 diabetes (T1D) and eliminate the need for insulin.
Nearly one in three Canadians are affected by diabetes. T1D is a chronic condition where the body attacks and destroys the insulin-producing islet cells in the pancreas. As a result, people with this disease produce little to no insulin, the hormone responsible for regulating blood sugar.
The Ajmera Transplant Centre is the largest and most successful transplant program in North America, one of the top three transplant research centres in the world and a leader in pancreas transplantation. This procedure requires major surgery, so clinicians are very selective about who qualifies.
“For patients that aren’t eligible for pancreas transplantation, we look to do islet transplantation,” says Dr. Reichman.
In this procedure, functional, insulin-producing islet cells from deceased donors are transplanted into people living with T1D to replace the islet cells that have been damaged or destroyed by the immune system. Once transplanted, the cells can secrete insulin and regulate blood glucose.
“The beauty of islet transplantation is that it’s really one of the most minimally invasive operations that we can do,” says Dr. Reichman.
However, islet transplant also comes with disadvantages.
“The outcomes from islet transplantation at this point don’t come close to matching the outcomes from pancreas transplantation,” says Dr. Reichman.
A lack of available donors and the need for immunosuppression afterward also add to the challenges of islet transplantation. This is where the McEwen Stem Cell Institute comes in.
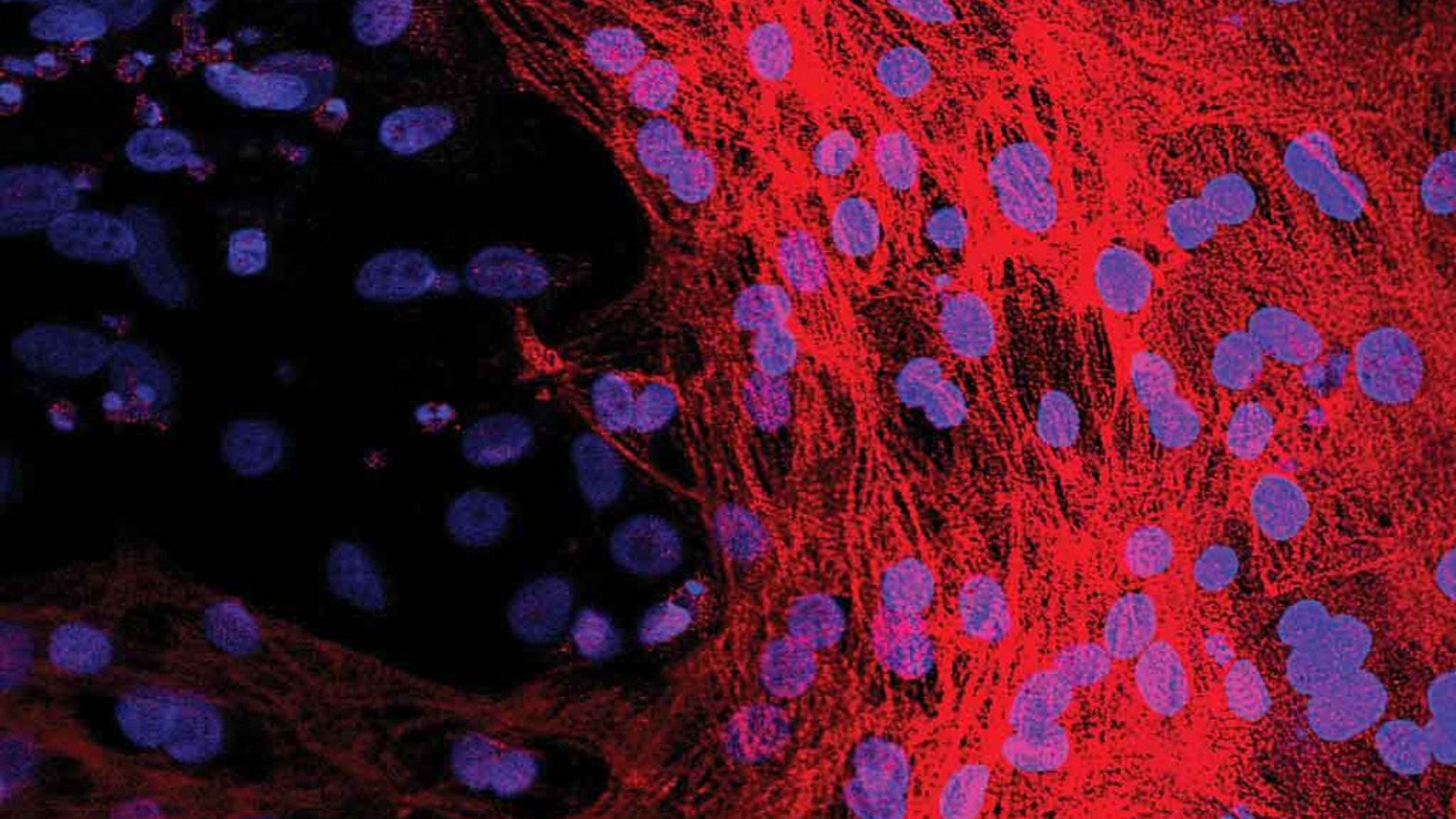
“The dream that we have as stem cell scientists is that we can actually create a surrogate islet that we will be able to transplant without immunosuppression,” says Dr. Nostro.
She has been working for years to develop insulin-producing cells from stem cells that can be transplanted into people with diabetes to replace the insulin-producing cells that have been destroyed by the immune system. This process has included using genetic engineering to make the cells invisible to the immune system.
“Then you could potentially have a source of islets that come from stem cells so it would be unlimited. So you don’t have to worry about looking for the perfect match or looking for the right donor,” says Dr. Nostro.
She has made incredible progress, demonstrating that her cells can regulate blood sugar in animal models.
The downstream impact of this work could be life-changing for those with T1D. These advances would eliminate the daily burden of monitoring blood sugar and administering insulin and limit the risks of life-threatening diabetes-related complications.
Vanessa Oliver was diagnosed with T1D at age six. During the presentation, she shared what these innovations mean to her.
“I can’t express enough how much I crave getting a chance to live life without the mental toll of type 1 diabetes,” says Vanessa. “I mean, hopefully, my smile says it all. I really have been a believer since day one that a cure is there to be found.”
Now comes the hard part – getting the insulin-producing cells from Dr. Nostro’s lab to patients.
“Our long-term goal is really to collaborate with the Ajmera Transplant Centre to launch a clinical trial here in Toronto,” says Dr. Nostro.
“Being one of the largest transplant centres, we have access to lots of patients that are really in need of a transplant,” says Dr. Reichman.
Now, they’re raising funds to build a team that will be able to bridge their work, optimize the transplant process and condition and improve the outcomes of islet transplantation.
Dr. Reichman sees this as an exciting opportunity.
“We all love to take care of patients, but I think many of us also want to see and want to improve on how we take care of patients and we can’t do that without research,” says Dr. Reichman.


