A national initiative that helps patients with reduced access to transplants find a matched donor is celebrating its 1000th kidney procedure, a milestone made possible by experts and technology at UHN.
Canadian Blood Services announced on Thursday, July 25 that the Highly Sensitized Patient (HSP) Program has reached 1,000 kidney transplants a little more than a decade after the initiative was launched. Of those, 98 were performed at UHN’s Ajmera Transplant Centre.
“That’s 1000 patients who likely otherwise would have had a much lower chance of ever receiving a transplant,” says Dr. Kathryn Tinckam, UHN Physician in Chief, former Director of the Histocompatibility (HLA) Laboratory at UHN, and former Medical Director of the National Transplant Registry, which has been operating the HSP Program since 2013.
Highly sensitized patients are medically suitable for a kidney transplant but have an immune system profile that makes it much more difficult to find a matched donor organ. They usually wait longer for a transplant than less sensitized patients and are more likely to become ill or die while waiting.
There are three main risk factors that increase the chance of a patient becoming highly sensitized, Dr. Tinckam says: having had a prior transplant, having had a blood transfusion, or having been previously pregnant.
Approximately 20 per cent of patients on provincial waitlists are highly sensitized and in need of a kidney transplant, according to Canadian Blood Services.
Largest laboratory of its kind in Canada
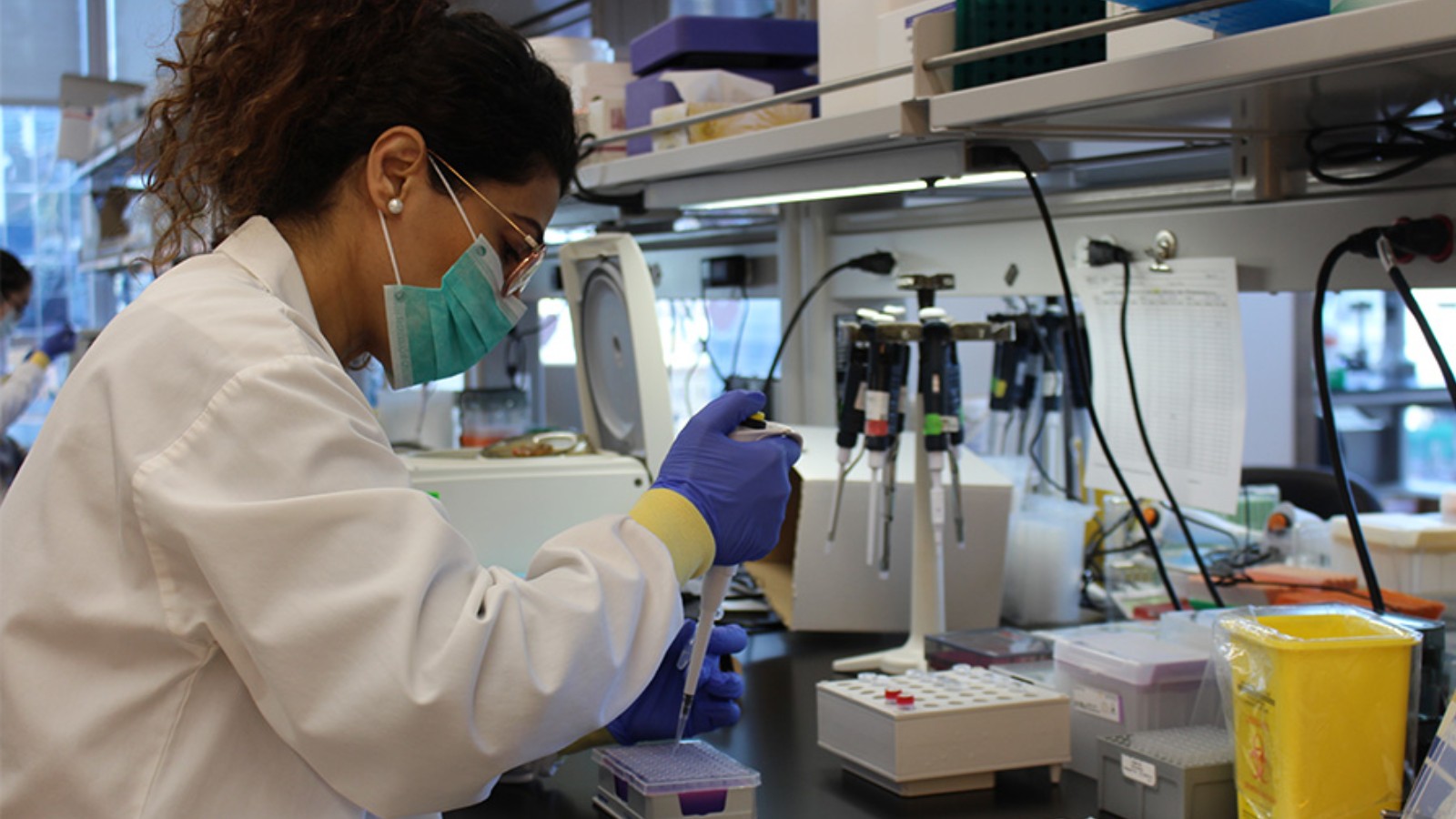
The HSP Program gives these patients access to a wider pool of kidney donors by registering provincial donor information into a shared national organ allocation system, which increases the chances of recipients finding a suitably matched donor. HLA laboratories across the country are responsible for doing extensive donor DNA testing, recipient antibody testing and compatibility tests for these patients on their waitlists.
UHN’s HLA Laboratory, part of the UHN Laboratory Medicine Program, is the largest of its kind in Canada — conducting immune testing and organ matching for patients being assessed and transplanted at centres in the Greater Toronto Area — and has been foundational to the success of the HSP Program.
“It’s local testing, entered in a national system to facilitate a shared algorithm,” says Dr. Tinckam, who played a major role in the establishment of national testing protocols.
Dr. Tinckam emphasizes the work of all HLA laboratories and clinical programs in Canada who came together to establish a sharing program and define best practices to support all patients in the country.
“Transplants are generally managed provincially, but when it comes to patients who are in the most need — those who have the hardest time accessing a donor — then we consider Canada to be the village that we work in.”
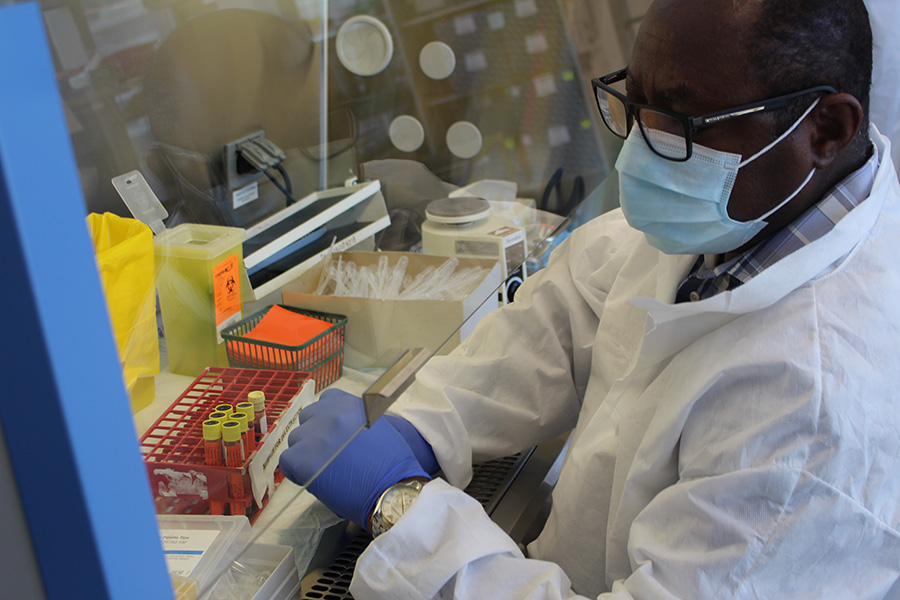
Dr. Jinguo Wang, Director of the HLA Laboratory at UHN, says being able to find these patients a donor from anywhere in the country is the most rewarding part of the job.
“It’s very exciting. Every time we find a compatible donor, I feel so thrilled for the patient,” says Dr. Wang, emphasizing that such patients would likely have been on a waiting list for the rest of their lives, or even died while waiting.
“Each transplant is one less patient on dialysis, and one more life that will significantly improve.”
There are more than 4000 people in Canada waiting for a transplant, according to Canadian Blood Services, approximately 3000 are waiting for a kidney. Every year, 250 Canadians die waiting for an organ transplant.
Cross-Canada collaboration
Dr. Edward Cole, former Physician-in-Chief at UHN and former Chair of the Canadian Blood Services Kidney Transplant Advisory Committee, which oversees program operations, policy and outcomes, says this milestone is a crowning achievement for the Canadian transplant community and a true testament to the power of teamwork.
“It’s an opportunity to show people how successful we can be when we work together and how technology has advanced to the point where we can standardize this process across labs throughout the country,” says Dr. Cole, noting there was little to no collaboration before these registries were set up.
One of the first steps in cultivating collaborative relationships between transplant programs, committees, registries and advisories across Canada was through the development of the Kidney Paired Donation (KPD) Program — a precursor to the HSP Program. Dr. Cole was a driving force behind it, and was previously recognized for that work through his recent appointment to the Order of Canada.
The KPD achieved its 1000th transplant milestone in 2023.
“Receiving a transplant is a truly life-changing procedure,” Dr. Cole says.
“It can give a patient the opportunity to do all the things that are most important to people in life – spending time with family, having a partner, having children, being able to travel.
“I’m very gratified by the work we’ve done and everything we’ve accomplished,” adds Dr. Cole, who calls Canadian Blood Services “a great partner” in championing these programs.
‘Level the playing field for highly sensitized patients’
Dr. Deepali Kumar, Director of UHN’s Ajmera Transplant Centre, calls the milestone “an incredible accomplishment that shows the impact of a highly dedicated kidney transplant team working together with the HLA laboratories on a national level.
“Organ donation is a remarkable act of heroism,” she says. “We couldn’t do this without the generosity of our organ donors.”
While there are now 1000 patients whose lives have been changed thanks to the collaborative work of Canadian Blood Services, and the HSP Program, HLA laboratories and transplant programs, there are still many more on waiting lists hoping to find a match.
Drs. Cole, Tinckam, Wang and Kumar hope this milestone will inspire more people to consider registering their intention to be an organ donor, or to consider learning more about living organ donation.
“What we’re trying to do here is level the playing field for highly sensitized patients, but it’s a number game,” says Dr. Tinckam. “The harder it is to find a donor, the more donors there needs to be.
“None of this would be possible without donors and their families.”
By Shauna Mazenes

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.


