
What is the best course of action to prevent and treat complications following transplant procedures?
Researchers at Toronto General Hospital Research Institute (TGHRI) helped answer this question by identifying the risk factors for kidney dysfunction that can occur after heart transplant, as well as the optimal clinical management strategies for this complication.
To investigate this, Dr. S Joseph Kim, clinician scientist at the TGHRI worked with students of the Multi-Organ Transplant Student Research Training Program (MOTSRTP).
The MOTSRTP, co-directed by Dr. Kim and Olusegun (Segun) Famure, research associate at TGHRI, is a unique, integrative student program that has been running since 2009. Organized by UHN’s Ajmera Transplant Centre, the program trains students in the foundations of clinical research through research-oriented projects.
“Our program allows students from all levels of post-secondary education – undergraduate, graduate or professional – the opportunity to gain exposure to the clinical and research components of organ transplantation” says Segun. “Students do hands-on research, write abstracts and manuscripts and present at scientific conferences.
“Since the program started, our students have been the first-author on 28 publications, co-authors on 20 more, and have submitted over 80 conference abstracts.”
In this study, students of MOTSRTP analyzed the risk factors and patient management strategies for chronic kidney disease in 291 Canadian adults following heart transplant.
“Heart transplant patients are at a particular risk of kidney deterioration due to need to take life-long immunosuppressant medications,” says Dr. Kim, who is also an associate professor in the Department of Medicine at the University of Toronto and the Director of the Kidney Transplant program at UHN.
“These medications are necessary to prevent rejection of transplanted tissue but can cause reduced blood flow to the kidney, scarring and other renal tissue damage.”
Recent studies suggest that additional risk factors for kidney disease post-transplant include increasing age, female sex, pre-transplant kidney function, blood pressure and blood sugar.
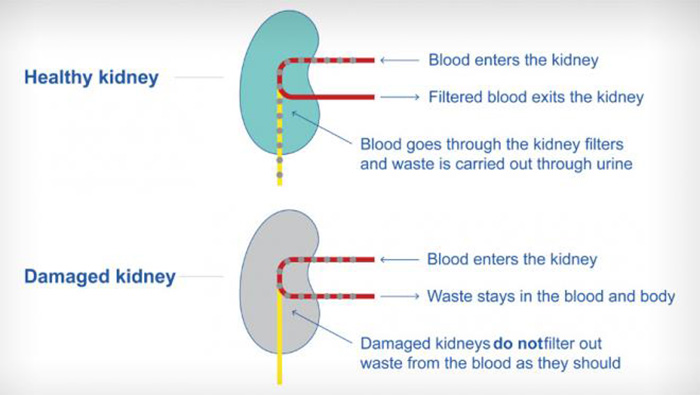
Chronic kidney disease represents a gradual loss of kidney function, which leads to improper excretion of bodily waste and electrolytes. It can progress to kidney failure which often requires dialysis, or even transplant.
“To determine the best way to manage transplant patients and improve outcomes, we wanted to validate the risk factors associated with renal dysfunction in the Canadian population and analyze current clinical management methods,” says Cavizshajan Skanthan, first author of the study and a student in the MOTRSTRP.
“We found that the factors associated with moderate to severe kidney dysfunction were female sex, older age, longer time since transplant and low kidney function pre-transplant,” says Jonathan Wang, co-author of the study and MOTRSTRP student.
“In addition, prescribing medications called mTOR inhibitors and withholding ones called calcineurin inhibitors were associated with kidney dysfunction,” says Imindu Liyanage, fellow author and student.
However, the research team cautions that further studies are needed to determine the effect of switching from calcineurin to mTOR inhibitors as patients are often switched to the latter when kidney function starts to decline.
“This study also showed that more patients should be referred to a nephrologist,” says Kristiana Xhima, co-author and student. “While referral to a nephrologist can help patients with kidney management and prevent further deterioration, only 19.7 per cent of patients showing signs of moderate-to-severe renal dysfunction were referred.”
The findings from this study will contribute to the knowledge of how to care for heart transplant patients at risk for kidney disease, says Segun.
“Thanks to the students in our MOTRSTRP program, we have been able to provide more evidence of the kidney disease risks and post-transplant practices to the medical community,” he concludes.
This study was supported by generous donors to UHN Foundation.


