By Bryan Borzykowski
If you find yourself at the Peter Munk Cardiac Centre over the next few years, don’t be surprised when you’re treated by a physician and their artificially intelligent tech. Soon, clinicians will be armed with devices that can tap into billions of pieces of information and provide care recommendations, in real time, that are highly specific to your situation. Artificial intelligence (AI) – computing systems that can process endless amounts of information to come up with answers to questions humans could never solve on their own – will help physicians provide even better care than they do now.
Dr. Barry Rubin, Medical Director and Chair of the Peter Munk Cardiac Centre, recognized long ago that for the Peter Munk Cardiac Centre to remain an innovation powerhouse, it needed to create an in-house AI team dedicated to advancing cardiovascular care – and it’s one of the few medical institutions in the world that’s taken this step. We spoke with Dr. Rubin and the AI team – Dr. Chris McIntosh, scientist at the Peter Munk Cardiac Centre and UHN’s Techna Institute, and Dr. Bo Wang, lead of the Peter Munk Cardiac Centre’s AI program – about how this technology could transform patient care.



Illustrations by Kyle Scott
How will AI be a partner in patient care?
Dr. Rubin: AI algorithms won’t replace the judgment of physicians and nurses, but they will help them make better decisions by giving them more access to information and by knowing how to interpret that data. The challenge is to roll out the use of AI in a safe way, which is another reason we have the computer scientists and physicians working together in-house.
Dr. McIntosh: A clinician could have an app on their phone with AI that’s making suggestions as to what kind of care to provide – they can interact with it, just like they do with their colleagues.
What are some of the problems you’re solving?
Dr. Rubin: The first is personalizing patient care. Imagine if you had two patients with the same disease, like a narrowed heart valve. If you knew everything about the patients, including their genetic information, you could use AI to predict the best treatment for each patient. The second is discovery science. Last is efficiency of hospital operations. We know how many patients we have in the intensive care unit today, but can we accurately predict how many it will have tomorrow? That’s important for running a hospital. We have more than two million patients in our database and hundreds of terabytes of information. Humans can’t make sense of all that information. With a machine-learning approach, we can look at the data and see if specific diseases are associated with certain genes or features on the heart ultrasound or in studies. This can lead to new research that explores why diseases happen, which is the first step in identifying new treatments.
Which projects are you focused on?
Dr. Wang: We’re working on a lot of projects, including one with Dr. Douglas Lee, who has collected clinical and molecular data from patients with heart failure – a disease that affects more than one million Canadians. He wants to know if we can use that data to predict the likelihood of readmission to hospital within the first 30 days after surgery. If we know the answer to that, we can design better treatments to provide better care for patients with heart failure and improve their quality of life.
Dr. McIntosh: I’m involved in surgical planning for interventional cardiology, working with Drs. Rubin, Heather Ross and Sanjog Kalra. When clinicians must identify blockages in the heart,
a catheter needs to be threaded into the patient’s heart to inject a
contrast dye. A fluoroscopy system takes images of the arteries around the heart and then looks at how the blood is moving. Usually, physicians view those images themselves to determine whether someone needs a balloon or surgery. We’re building AI to analyze pictures in real time, which will help cardiologists rapidly and accurately interpret heart X-rays, which will lead to better treatment choices.
Dr. Rubin: I’m excited about gene therapy. Maybe we find that someone’s heart is contracting in a certain way or the orientation of one of their heart valves is different because it’s associated with one gene – or maybe 46 genes. We have the opportunity to advance research into health care and science very rapidly, and there are few hospitals in the world that can do that.
Why is the Peter Munk Cardiac Centre the place to push the AI envelope?
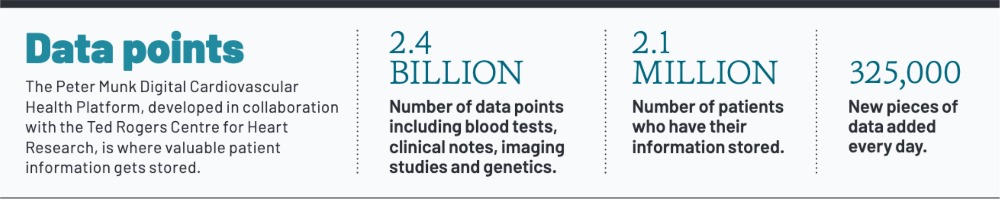
Dr. Wang: We have an amazing culture of collaboration that allows physicians and AI researchers to work together. Our Peter Munk Digital Cardiovascular Health Platform (DCHP) allows us to collect billions of data points, including blood tests, clinical notes, imaging studies and genetics, which we need to create AI models. The DCHP is one reason I chose to work here after I graduated from Stanford.
Dr. McIntosh: We’re in Canada’s largest and most multicultural city, so we have diversity. Other places don’t have a healthcare system that ensures equal access for everyone. So our data, and the models we create, are less likely to be biased. It’s a phenomenal place to be.
Dr. Rubin: We want to develop treatments that are used around the world. The key to that is AI. It has enormous, even limitless potential to deliver much better patient outcomes. We’re leading the way. I’m excited to be part of the future of this field and to see what it can offer patients.
This article originally appeared in the 2021 Peter Munk Cardiac Centre annual report. Read it here.


