[L-R] Dr. Hance Clarke is teaching patients how to live with their pain using alternative therapies. Dr. Anuj Bhatia is using technology to help patients track and manage their pain. (Photo: Regina Garcia)
By Anna Sharratt
If anyone knows how difficult it can be to deal with unrelenting chronic pain, it’s Paul Ross, a Toronto resident with colitis and Crohn’s disease who has been dealing with extreme abdominal pain for more than two decades. “It’s excruciating,” says Ross, who suffers from intestinal blockages multiple times a month. “There were times I didn’t want to live.”
Since 1989, Ross has undergone 12 operations. He has an ileostomy bag and, at times, has needed tube feeding. To control his pain, he’s relied heavily on powerful opioids. Unfortunately, relief came at a terrible cost: the side effects impacted his day-to-day life. “My kids were afraid that my grandkids would see me injecting myself,” he recalls. “Though everything was prescribed by my doctors, I had become a drug addict.”
The turning point came in 2016, when Ross developed sepsis, a life-threatening full-body infection. After an operation to remove damaged tissue, he was given two fentanyl patches, in addition to his self-injected hydromorphone for pain relief. That was when he realized he couldn’t live without powerful painkillers – and something had to change. “I told my doctor, ‘I’m not leaving here until I get a referral to someone who can get me off these drugs,’” he says.
His doctor knew who could help: Dr. Hance Clarke, a clinician investigator at the Krembil Brain Institute (KBI), an anesthesiologist and Director of Pain Services at the Department of Anesthesia and Pain Management and the Director of the GoodHope Ehlers-Danlos Clinic at Toronto General Hospital. That referral would transform his life.
A holistic approach
Dr. Clarke is a leading expert in opioid alternatives. He uses holistic therapies, such as mindfulness training, acupuncture, yoga, massage therapy, exercise and cannabidiol (CBD, found in cannabis), in addition to, or in lieu of, the powerful painkillers chronic pain patients take. These integrative approaches teach patients alternative strategies to control how they handle and experience their pain. “Your brain is as strong as your medications,” says Dr. Clarke. “We can teach patients how to live with their pain.”
In 2014, he created the Transitional Pain Service (TPS) at University Health Network (UHN), a one-of-a-kind centre that’s revolutionizing pain management by helping patients manage their pain and by preventing the development of persistent opioid use and misuse. Patients are either directed to the clinic after surgery – they may have pain out of the norm and are prescribed opioids – or are already taking medications and need guidance regarding pain and medication management.
Many doctors still prescribe opioid medications after routine medical procedures and, for those who go on to develop a problem related to their care, the TPS enables support during this challenging time. One in 10 patients on high-dose opioids eventually struggles with an opioid misuse problem. “We’ve created a template for institutions to help these patients earlier in their post-operative pain trajectory so they don’t go on to develop an opioid use disorder,” says Dr. Clarke.
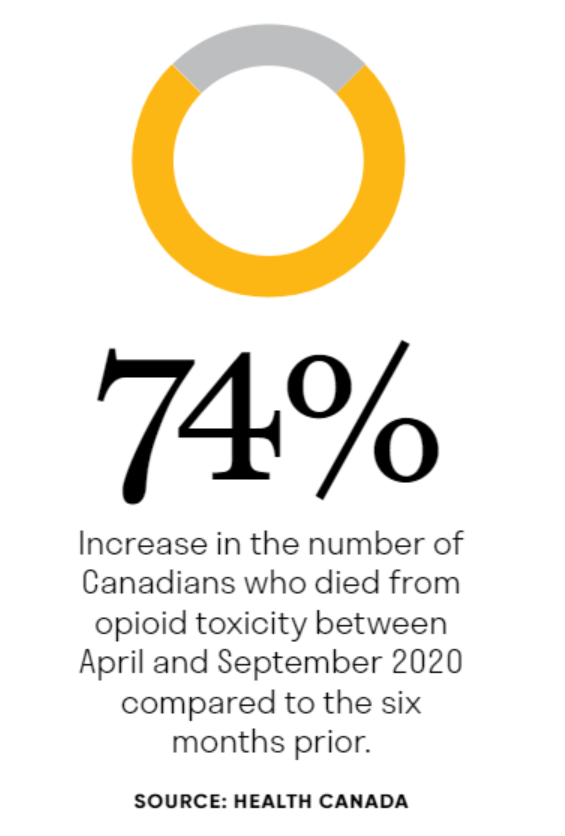
From April to September 2020, 3,351 Canadians died from opioid toxicity, a 74 per cent increase from the six months prior, according to Health Canada. The increased use of fentanyl-like substances continues to be the main culprit for these deaths, and patients on high-dose opioids need a safe place to turn. The TPS practises a non-judgmental approach that supports some of the most vulnerable patients.
Ross’s withdrawal was challenging. He went to the hospital for medical support, but when he got there, he was too weak to stand. “I was constantly throwing up,” he says. “Dr. Clarke carried me to the bathroom in his arms.” Dr. Clarke prescribed him suboxone, an opioid agonist treatment medication, which helps relieve the debilitating symptoms of withdrawal. He also checked in with him constantly, even phoning him at home. Just one day after starting suboxone, Ross could see progress. “I woke up, showered and suddenly realized: not once did I reach for my syringe,” he says.
In the weeks that followed, Ross tried acupuncture, yoga and therapy under Dr. Clarke’s guidance. But it was the centre’s mindfulness program with Dr. Aliza Weinrib – using breathing exercises and guided imagery to bring awareness to the present moment – that gave him the tools to start his new life. “Now I can respect my pain – I’m not scared of it,” he says.
Drug-free digital advances
In addition to employing holistic approaches, the TPS launched a digital health app to help patients monitor pain symptoms and improve their contact with clinicians. Patients rank their pain scores out of 10, document their emotional reactions and provide summarized reports of their progress. “People who used the app reported a reduction in anxiety and catastrophizing,” says Dr. Anuj Bhatia, a clinician investigator at the KBI and Director of Anesthesia and Chronic Pain Clinical Services at UHN.

There have also been advances in drug-free techniques such as neuromodulation, which is the use of devices that generate electrical currents to override pain signals from nerves. Patients can control the intensity of the device, depending on their pain. “It is quite an amazing therapy, as it allows patients to come off opioids,” says Dr. Bhatia, adding that other drugs, such as ketamine, an anesthetic medication, are also being explored as a way to help patients with long-term neuropathic pain.
Patients aged 16 to 80 have benefited from these implants at the Neuromodulation for Pain Program at UHN. Other image-guided interventional procedures performed at UHN have also helped alleviate certain types of pain originating in the spine or the nerves. For instance, in 2019, Terie Elliott, a patient in the program, received Canada’s first battery-free peripheral nerve stimulator to alleviate intractable foot pain. She’s now walking, bending and moving.
Physicians, nurses, psychologists and physical therapists in the Comprehensive Integrated Pain Program at UHN, in collaboration with pain programs at Sinai Health and Women’s College Hospital, have also created clinics to address other kinds of pain, whether it’s related to joints and muscles, headaches and facial pain, cancer or pregnancy.
As for Ross, he is no longer on any pain drugs and practises mindfulness whenever he experiences an intestinal blockage. “I was the world’s greatest skeptic,” he says. “But it’s unbelievable what mindfulness has done for me. I have my life back.”


