Eric Celentano is more active than ever thanks to the Ex Vivo System-treated lungs he received at the Ajmera Transplant Centre. (Photo: Tim Fraser)
By Diane Peters
Eric Celentano thought the pesky pain in his shoulder that began in summer 2012 was from playing golf, his favourite sport. He figured some physiotherapy would fix the issue, or, at worst, he’d need to take a few weeks off. But instead, X-rays of his shoulder revealed something far more troubling than tendonitis: a serious lung condition called idiopathic pulmonary fibrosis (IPF). “I was selling respiratory equipment, so I knew what was going on when I received the diagnosis,” recalls Celentano, who’s now 64. “But I was scared of what was to come.”
He knew that IPF – a progressive disease that causes the lungs to become scarred and stiff over time – could kill him and that his only chance of survival was getting a double-lung transplant.
Celentano’s lungs did gradually become worse, and eventually the antifibrotic medication he was on wasn’t helping anymore. “By the summer of 2018 I couldn’t swing a golf club or even walk up the stairs,” he recalls. Celentano needed oxygen whenever he exerted himself, which was depressing for someone used to being busy and active.
In the fall of 2018, with his health in serious decline, a pair of lungs became available. Celentano was prepped for surgery at Toronto General Hospital. However, his surgeon, Dr. Marcelo Cypel, Surgical Director of the Ajmera Transplant Centre at University Health Network (UHN), wasn’t sure if the lungs were healthy enough to save Celentano’s life.
Fortunately, Dr. Cypel, who is also part of the Sprott Department of Surgery at UHN, had been part of the team that developed a device more than a decade ago that is able to test and even repair injured donor lungs. It’s called the Toronto Ex Vivo Lung Perfusion System, a dome-shaped incubator-like machine that lets organs live outside a body for many hours. Tubes, pumps, ventilators and filters send liquids, oxygen and nutrients into the lung, keeping it alive and allowing it to essentially breathe in and out. While only a few centres around the world have such a device, Dr. Cypel and the Toronto Lung Transplant Program team at the the Ajmera Transplant Centre now use it as their standard of care to assess donor lungs for transplantation.
The first pair of lungs weren’t healthy enough, but several weeks later, Dr. Cypel received lungs from a donor who had passed away from a sudden cardiac arrest. Normally in this situation, lungs aren’t suitable for transplant, as they get starved of oxygen and blood for hours while donation is arranged. But Dr. Cypel was leading a new research program for organ donation after cardiac death, which uses the Ex Vivo System to make them ready for transplant.
Like he did before, Dr. Cypel tested the lungs in the Ex Vivo System, and this time they were good to go. Six months later, Celentano was back on the golf course, and a year later, he completed the famed Grouse Grind, a steep hike up Grouse Mountain in North Vancouver. “I didn’t just get back to life – I went back to a better life,” he says.
20%
-Source: JAMA Surgery
Approximate mortality rate of those on the wait list for a lung transplant.
30%
-Source: UHN
Approximate percentage of deceased donor kidneys that do not work immediately.
Modern-day miracle
The Ex Vivo System – which was co-developed by Dr. Shaf Keshavjee, Surgeon-in-Chief of the Sprott Department of Surgery at UHN, and Dr. Cypel – is nothing short of a modern-day medical miracle. If a damaged organ can be kept alive outside a body, where it can then be treated with medications and other procedures to essentially become as good as new again, then the number of organs available for transplant can increase exponentially. That’s a huge deal. Canada has a shortage of organs – in 2019 alone, 249 people died while waiting for a transplant.
In 2006, Dr. Keshavjee wanted to research how to alter some of the genetic components of lungs to make them healthier, and knew it would work best on organs kept warm and moist outside the body. Ex vivo technology was aspired to for decades, but no one had gotten it right just yet. “We put the pieces and the physiological concepts together,” recalls Dr. Cypel. He and Dr. Keshavjee oversaw the world’s first transplant of Ex Vivo System-treated lungs in 2008 at UHN. Not long after, the Ajmera Transplant Centre fully doubled the number of lung transplants it performed each year. “It transformed the field of transplantation,” says Dr. Cypel.
With the Ex Vivo System, “we can assess an organ’s function in detail, so you can make sure it’s going to work after you transplant it,” explains Dr. Keshavjee, who is also the James Wallace McCutcheon Chair in Surgery, Director of the Toronto Lung Transplant Program at the Ajmera Transplant Centre and Director of the Latner Thoracic Surgery Research Laboratories at UHN. “We pioneered this approach with lungs and demonstrated how to use it. Now, it’s been translated around the world to increase lung transplant access and is being extended to other organs.”
Organs such as the kidneys and liver have their own version of the Ex Vivo System, too, and devices for the heart and pancreas are in development. While they essentially function in the same way, they all look a little different, as each organ needs different supports – including the type of liquid used to keep them going – and are at various stages of development.
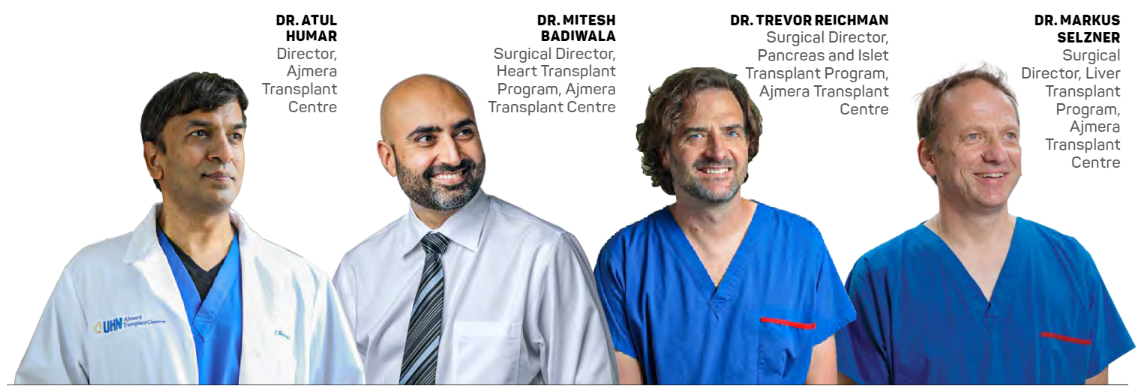
“Livers get damaged during the regular preservation process. When they’re cooled, they have no oxygen and they become less healthy,” explains Dr. Markus Selzner, Surgical Director of the Liver Transplant Program at the Ajmera Transplant Centre, who is also part of the Sprott Department of Surgery at UHN. He started his own ex vivo research nearly 10 years ago. The device allows doctors to see if the liver can make bile and blood clotting factors, and metabolize toxins. If it can pull off these key functions, it’s likely the organ can be successfully transplanted.
For nearly a decade, there have also been devices that support hearts, but Ajmera Transplant Centre clinicians are trying to improve upon what’s out there. “What exists now has allowed us to take hearts that have stopped and restart them outside the body,” says Dr. Mitesh Badiwala, Surgical Director of the Heart Transplant Program at the Ajmera Transplant Centre, who is also part of the Peter Munk Cardiac Centre and Sprott Department of Surgery at UHN. “But these devices have limitations. They just keep the heart alive. We want to develop an actual Ex Vivo System to be able to test heart function and repair hearts prior to transplantation.”
He’s collaborating with engineers to create a more powerful Ex Vivo System that makes all of a heart’s chambers pump blood – like they do inside a body – which will allow him to test its ability to fully function. He also wants to keep hearts in the device for longer (the current time limit is four hours) so he’s working on ways to feed the heart nutrients and clear it of toxins.
Researchers at the Ajmera Transplant Centre are also developing ex vivo protocols for the pancreas. “The pancreas is a pretty angry organ,” admits Dr. Trevor Reichman, Surgical Director of the Pancreas and Islet Transplant Program at the Ajmera Transplant Centre, who is also part of the Sprott Department of Surgery at UHN. “It doesn’t like to be manipulated at all, let alone be transplanted.” This organ easily develops inflammation or “pancreatitis,” so he’s working on a system that calms it down and inactivates some of the enzymes that cause inflammation.
An Ex Vivo System for kidneys is also on the way, to kick-start the organ into operation after coming out of cold storage. “Sometimes the kidney is extremely slow to start working after a transplant,” notes Dr. Reichman.
More ex vivo innovations
Hours in a device are great; days are even better. Dr. Cypel and his team in the Latner Thoracic Surgery Research Laboratories recently hit a record three days of preserving lungs in the Ex Vivo System. They did it by alternating cold preservation at 10ºC instead of 4ºC, which slows down the organ but does not shut it down entirely. The lungs are then placed in the Ex Vivo System at body temperature for four hours, to recover and recharge, and then back to cold again for about 18 hours. This process keeps the lungs from needing too many nutrients and extends their ability to live outside the body. Dr. Keshavjee alludes to where this research is leading, “One day, I’m hoping we can have organs on the shelf, so you just go in and get what you need when you need it.”
Meanwhile, innovations in ex vivo technology may help imperfect organs improve. Already, the lung team has removed blood clots from organs and treated them with antibiotics. With livers, overweight donors may have organs with a slow fat metabolism. “We’re working on research to increase the metabolism of livers,” says Dr. Reichman. “We might be able to increase the fat burning of the liver while it’s on the Ex Vivo System.”
Many organs also harbour infections and viruses that can be removed ex vivo. “We give transplant patients anti-rejection medications, which severely knock down their immune system. So, any minor infection can become pretty life-threatening,” says Dr. Atul Humar, Director of the Ajmera Transplant Centre and the R. Fraser Elliott Chair in Transplantation Research. “If you can take the virus out of the organ before it even gets to the recipient, then that’s a major advance.”
Already, Dr. Humar and his team have shown that a short course of antivirals can eliminate hepatitis C in donor organs. Next, researchers are figuring out how to treat organs for Epstein-Barr virus and cytomegalovirus – a virus that is common but usually harmless in the general population, but can be a dangerous infection in transplant recipients.
“We pioneered this approach with lungs and demonstrated how to use it. Now, it’s been translated around the world to increase lung transplant access and is being extended to other organs.”
— Dr. Shaf Keshavjee
An ambitious future
Drs. Cypel and Keshavjee’s long-term plan is to use the Ex Vivo System to help physicians engineer better organs. It’s years away, but clinicians may be able to change the blood type of an organ so the sickest people can get access to the next available organ instead of waiting for the one that exactly matches their blood. “We could make a universal organ,” Dr. Cypel says.
Going back to the idea that inspired the Toronto Ex Vivo Lung Perfusion System years ago, Dr. Keshavjee is working on gene therapy to stop an organ from being attacked by its new host. “We could make the lung look more like ‘self’ and prevent rejection,” he says. This could reduce the risk of transplant failure and, with patients taking fewer anti-rejection drugs or none at all, lower their infection risk and improve their quality of life.
Already, the Ex Vivo System has saved countless lives like Celentano’s. “In 10 years,” says Dr. Keshavjee, “Ex vivo organ perfusion will be the standard of care everywhere.”