
Randall Cote is regaining some independence one conversation at a time.
In 2017, he was in a motorcycle accident that left him in a coma and paralyzed from the waist down. After weeks in acute care, he was pre-emptively taken off 24-hour support.
Soon after, Randall suffered a heart attack, which he survived after nearly six minutes of CPR. That led to a diagnosis of Lance Adams syndrome (LAS), a rare condition resulting from extensive brain damage due to cardiac arrest.
One of the complications for patients with LAS is trouble speaking.
But the Augmentative and Alternative Communication Clinic (AAC Clinic) interdisciplinary team at Toronto Rehab‘s Bickle Centre prescribed Randall an assistive technology device, allowing him to communicate.
“I would not leave the hospital without it,” Randall said through the device. “It enables me to clearly communicate with people when we are face-to-face.”
Care at the right place, right time
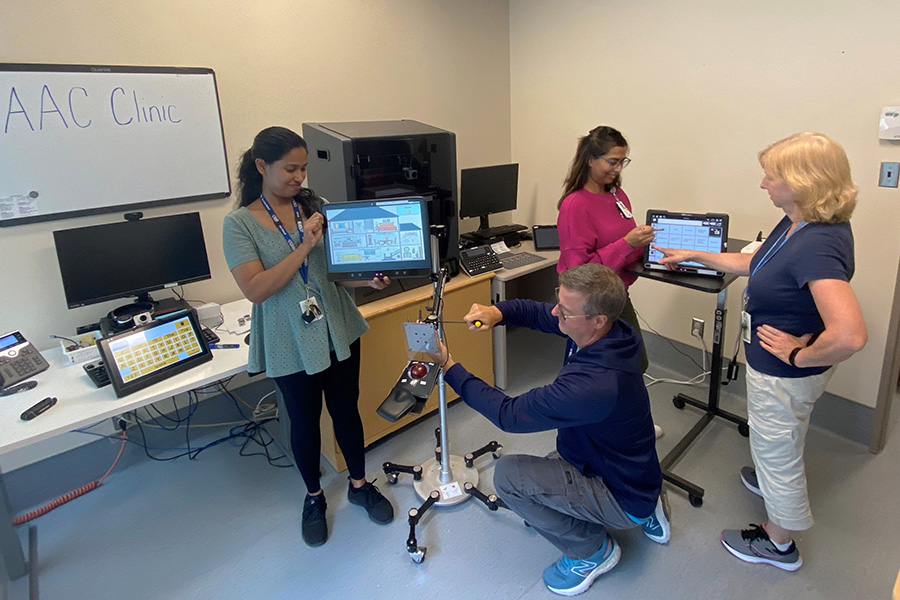
The AAC Clinic is unique to Toronto Rehab and serves both inpatients and outpatients across Ontario.
The team consists of an occupational therapist, speech-language pathologist, technologist and communicative disorders assistants passionate about working together and building on each other’s professional expertise to find solutions for communication barriers of patients.
Randall’s assistive technology is a Grid Pad 12 device that uses mouse access and looks like a typical tablet.
Working alongside Randall, the AAC Clinic team has figured out how to connect his device to email, Skype, and the internet, so he has access to everything he enjoys, all in one spot. He is also able to use the device both in bed and while sitting in his wheelchair.
While the device provides Randall with the ability to communicate his thoughts without requiring others to guess from non-verbal cues, he admits it doesn’t address all his frustrations.
“I’m interrupted all of the time because people try to finish my sentences,” Randall says. “I wish people would be more patient with the device and allow me to finish.”
However, even with these barriers, Randall says the device makes all the difference in his life, from talking to staff and family to ordering his morning coffee.
Harnessing the power of technology
Adity Roy, an occupational therapist in the AAC Clinic, explains how there are both physical and language factors that go into deciding what the best system for a patient will be.
“The possibilities are endless when you take into account combinations of different types of software and devices along with different access methods like switches, joysticks, mouse, headmouse, eye-gaze modules and more,” she says.
Most of the specialized devices come in the form of a touchscreen device that can be mounted to a patient’s wheelchair. Then, depending on their abilities the device can be adapted.
“We can use layouts that are picture-based for patients who have lost the ability to read,” she says.
“For example, there would be a picture of a house and after clicking it, different rooms in the house will be displayed. When the patient clicks on the bedroom and taps on the bed, it says, ‘I’m ready to go to bed.'”
Patients who don’t have use of their arms can use a head mouse, while eye-gaze technology allows patients to control their tablet.
Other devices, like Randall’s, are equipped with an on-screen keyboard that allows a patient to type out what they wish to say. After each word is typed, the computer will say it out loud. Built-in word prediction also helps make communication quicker.
Because Randal suffers from hand tremors as a result of his LAS, he has trouble using the touchscreen tablet or a physical keyboard. After multiple assessments, the team discovered he had best results using a mouse.
This diversity of devices means the AAC Clinic can continue to make adjustments as a patient’s needs evolves. For example, a patient with ALS might start with a touchscreen device accessed using hands, but progress onto a different device accessed using eye-gaze as their disease progresses.

But this advanced technology comes at a cost – devices can range from $3,000 to $20,000 – and it’s one that can pose a barrier for some patients.
Fortunately, the AAC Clinic has access to funding through the Government of Ontario’s Assisted Devices Program. That covers most of the costs, with patients paying the remainder through a monthly “rental” installment divided over five years of use. This fee can be up to $83 per month.
But the team can help with that, too.
“Patients with a fixed income, they have less flexibility,” Adity says. “We help them apply for funding assistance programs, like the March of Dimes, to ensure that even if they are facing financial strain, they have access to the best equipment possible.”
The AAC Clinic does not stop at initial assessments. Toronto Rehab is dedicated to ensuring patients and families have access to and are comfortable using technology throughout their journeys.
“We are constantly looking at ways to make a patient’s experience better and listen to what their specific needs are,” Adity says. “Each patient that comes through our doors has different needs, whether it’s financial, language, visual or physical.
“Our team is here to provide our patients with supports to help with communication and to improve their quality of life.”


