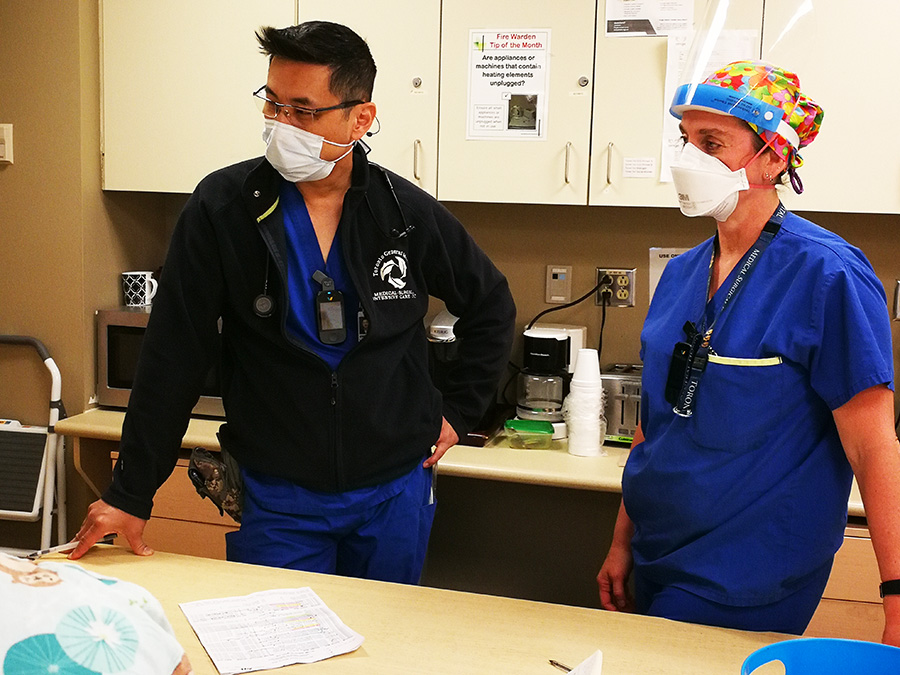
“It’s hard. You’re going in and you see somebody who’s dying. Very, very slowly dying, and it’s very distressing,” Toronto General Hospital MSICU physiotherapist Nathalie Coté says of the mental toll of the pandemic, now well into its second year. (Photo: UHN)
“We’ve been surrounded by death for a year-and-a-half.”
As Nathalie Coté says this, she is not holding back her tears.
The physiotherapist in Toronto General Hospital’s Medical Surgical Intensive Care Unit (MSICU) has watched too many patients die from COVID-19. For a healthcare worker, hard-wired to treat and heal patients, the grief and sense of helplessness is heart-wrenching.
“It’s hard,” she says. “You’re going in and you see somebody who’s dying.
“Very, very slowly dying, and it’s very distressing.”
The ravages of this pandemic are making it hard to reconcile her 20 years of experience working at the TGH MSICU and seeing the vast majority of her patients recover and go home.
The pandemic has thrown that success rate out the window. And the burden of seeing up to 40 per cent of patients die is not just weighing on her – it is crushing.
“Everything is on high alert. You start crying randomly,” explains Nathalie. “You have a bit of a meltdown and then you just pick yourself up and go again.”
In addition to an emotional toll, the pandemic is exacting new demands of her profession.
The TGH MSICU physiotherapy mantra is “early mobility” – moving joints to keep them loose and help retain muscle mass. Getting patients up standing, taking a few steps in their room, and then walking the hallway to promote lung function. Over the years, Nathalie has also employed outside-the-box treatment such as yoga, treadmills, and brief outings. All to promote recovery and get patients back to their daily lives.
“We’re physically training, strengthening the muscles,” Nathalie explains. “We’re strengthening your bicep, your erectors for example, which is strengthening the muscles of your back which will help with posture and help you to breathe better.
“If we rehab them early enough, we get them strong enough to get off the ventilator machine and we rehab them enough to go straight home from the floor. We assist in making the hospital stay shorter.”
But the coronavirus has drastically altered that trajectory. Patients who land in MSICU are the sickest of the sick. The 10th floor at TGH is the last stop for survival. Many are intubated, sedated, and on ECMO – the extracorporeal membrane oxygenation machine that does the job of the lungs to allow them to rest and recover from COVID-19. A portion of your blood gets siphoned off, passes through a circuit that removes carbon dioxide and infuses oxygen, then returns it back to your bloodstream through the another vein.
On this day, 24 of the 38 MSICU patients are on ECMO. That means Nathalie is often limited in what she can do.
“Our therapy is really minimal until they get out of that really dangerous zone, which sometimes takes weeks, even months for them to be medically stable enough for us to wake them up and then to start sitting him at the edge of the bed,” she says.

Starting at 7 a.m., the first hour of her day is listening to the night nurse recount the status of the 38 patients in MSICU. Following that, Nathalie and fellow physiotherapist, Vincent Lo, round the entire unit, one-by-one assessing each patient for treatment.
“He’s paralyzed, so he’s a no.”
“We can walk him.”
“Oh, he died.”
“I ranged him yesterday, but don’t touch the right leg.”
At 8:30 a.m., Nathalie and cardiovascular perfusionist, May Nguyen-Vu, are discussing the logistics of taking a non-COVID ECMO patient on oxygen for a “road trip.” Candice is a pregnant mother with pulmonary hypertension and in critical need of a lung transplant. The goal thus far has been to help keep both Candice and the baby healthy. The next decision is timing of the delivery and mom’s transplant. Candice was admitted to the MSICU and put on ECMO just 22 weeks into her pregnancy. She has not been outside the hospital since. That was 46 days ago.
For the last several weeks, Nathalie’s mission has been to keep Candice mobile and strong. She’s got her up and walking around the ICU, assisted with a walker, accompanied by staff wheeling all the paraphernalia and machinery needed to keep her alive. Later today, the plan is to help Candice get outside for some fresh air.
At the 9 a.m. MSICU unit huddle, Nathalie announces the road trip. Someone pipes up, “well, that’s a happy thing.” The entire group bursts into applause.

Next, Nathalie turns her attention to treatment. She dons her personal protective equipment and heads into the room of her first patient – motionless, intubated and on ECMO. As she approaches the bedside, she reaches out and takes his hand.
“Hello! It’s Nathalie. I’m the physiotherapist. Can you squeeze my hand?”
No response. This will be a bed exercise treatment, known as “ranging.” Nathalie gently, methodically and repeatedly moves and stretches the patient’s hands, arms, legs and feet.
The second patient is in much the same condition. Intubated, on ECMO and dialysis. As she moves each limb, Nathalie deftly navigates around and through the dozen or so lines of plastic tubing carrying blood and drugs and nutrients. Despite her being the one orchestrating the moves, she murmurs constant encouragement to the patient.
“Yes, that’s it… a little more… there you go.”
The next patient is on oxygen and ECMO, but more alert and mobile. He agrees to sit up. With Nathalie’s spotting him for balance and May manoeuvering his ECMO and IV tubing he turns so that his legs dangle over the side of the bed. She then lowers the bed, and with one hand around the back of his neck for support, asks the patient to lift his legs one at a time to a horizontal position. He shakily complies. After a few minutes, he resists further leg extensions. He wants to lie back down. Nathalie gets him back into bed and reverts to bed exercises for the rest of the session.
After each treatment, Nathalie sits down at the Nursing Station to enter notes into the patient record. Staff pass by while she writes, asking if the road trip is still happening.
“I can’t remember the last time we took an ECMO patient outside,” says one.
“And pregnant!” adds Nathalie.
For the next patient, it’s another case of ranging. In this session, Nathalie feels “crackling” in the lung area. She begins to pat and push the area vigorously with both hands to loosen whatever debris or fluid has built up. This helps clear the lungs and promote lung function.
At 11:30 a.m., Nathalie heads over to Candice’s room to begin preparation for the road trip. She is joined by May Nguyen-Vu and Candice’s MSICU nurse. They make a number of calculations, such as how long the ECMO will be on battery and how much oxygen will be needed. Candice is outfitted with a headband. The intravenous (IV) tubes are gathered up and tucked into the headband for safe keeping. The tubing flows like dreadlocks around her head to the IV pole.
A second nurse enters the doorway, carrying an extra cylinder of oxygen. Back-up for the trip. Next arrival is the doctor to oversee Candice’s condition throughout the walk. Finally, a chest high walker is brought in. Candice manoeuvers to the edge of the bed and reaches up to grab the walker. She wears a dressing gown in case it’s cool outside. Her husband Collin is at her side carrying a blanket.
“Ready Candice?” asks Nathalie.
“Oh ya!” she says.
The entourage-in-blue moves in careful lock step to ensure the myriad of tubing doesn’t kink or come loose. May wheels and monitors the ECMO machine. Beside her, Candice is on the walker with Nathalie close behind to spot her. Completing this line dance is the registered nurse wheeling the IV pole. Her husband, Collin, the doctor, and nurse carrying the oxygen all follow behind.
As the cavalcade moves down the hallway, staff stand clear, watching with masked smiles ear-to-ear. Some give encouragement. One asks, “going for some street meat Candice?!”

Everyone is pulling for Candice.
“There’s death here every day,” comments Nathalie later in the day, “That’s why people were so excited to see Candice go out today because it’s something good.
“It’s not somebody dying again.”
As they make their way to the elevator, the group must stop a few times to allow Candice’s oxygen saturation levels to get back above 92 per cent.
By 12:30 p.m., the ensemble has made it to the Elizabeth St. exit. Nathalie brings Candice a chocolate gelato. And, for the next 20 minutes, everyone sits. Basking in glorious sun. Not saying much. Happy for this brief respite from the grim reality inside.
“I feel good,” Candice says to everyone. “Thank you all for taking me out.”
For Nathalie, this moment is special. One of the small victories you savour.
“Those are fabulous and that’s what you gotta remember – you’re not going to lose all the time,” says Nathalie. “COVID’s making us lose a lot, but there are some battles that we are winning.
“They survive. There’s people that do survive.
“Today, brings you hope, brings you back to where it becomes exciting again to work here, to innovate and to make a difference to that person in life.”


