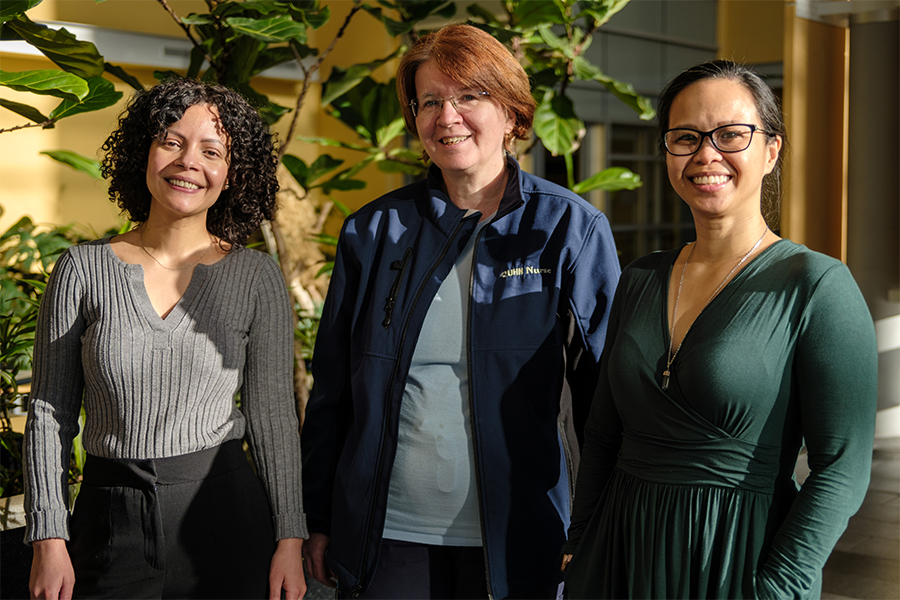
“We saw a clinical need for this type of care and realized for it to be sustainable, we needed an interdisciplinary team and an integrated care model,” says Dr. Adrienne Tan, staff psychiatrist and Medical Lead for the University Health Network’s Centre for Mental Health’s Medical Psychiatry Division. (Photo: UHN)
“We are helping clinicians and patients and families understand that there is a huge connection between their minds and their bodies,” says Shannon Wright, nurse practitioner in the Mental Health in Medicine Clinic (MHIM) at University Health Network (UHN).
“We’re not approaching health problems in just one way but recognizing that physical and mental health influence one another and go hand in hand.”
The Centre for Mental Health’s newest clinic aims to bring integrated care into action with low barrier access to psychiatric care for UHN patients receiving medical or surgical care.
UHN patients struggling with their mental health while getting outpatient care for a physical health condition can be referred to the clinic by a physician or nurse practitioner and get up to six months of treatment.
“The mental health impact of physical health issues is not regularly recognized or treated,” says Nicole Bangloy, the MHIM’s social worker. “It is very daunting and difficult to find mental health care and having a clinic within UHN where patients attached to medical clinics can be sent is important.”
Because care is provided at UHN, the clinic also helps improve the coordination of psychiatric and physical health care.
A similar service exists for UHN inpatients and those in areas such as Psychosocial Oncology or transplant. But until now, the only option for the rest of UHN’s outpatients was a referral back to their primary care provider or community services for mental health care. The new clinic allows timely access to psychiatric care – typically two to three weeks for first consultations – and helps UHN patients avoid potentially long wait times.
“We wanted to have a clinic that was open to all patients who are receiving medical and surgical care and needed mental health care,” says Dr. Adrienne Tan, staff psychiatrist and Medical Lead for the UHN’s Centre for Mental Health’s Medical Psychiatry Division.
Dr. Tan, along with a group of Centre for Mental Health psychiatrists, proposed the clinic, and with organizational support and a $1-million gift from the Slaight Family Foundation, it was quietly launched last year.

Fully staffed as of this spring, the clinic has worked with a wide range of patients, from age 18 to 85, with mental health concerns from mild to severe. Some have had their lives upended because of their health, and been unable to return to work, compounding poor mental health with financial stress.
Many report anxiety or low mood. The most frequent referral sources include General Internal Medicine, Rheumatology and Red Blood Cells Disorders.
The clinic has also seen a number of long COVID patients.
For some MHIM patients, it’s not about a new physical health condition, but the management of an existing, chronic condition. Some diseases – such as sickle cell anemia – can be painful and flare ups can last weeks or months. Patients may have anxiety about coping with new or increased levels of pain.
“Something just tips the scale and that’s what triggers the referral to our clinic,” says Shannon. “We know that in these conditions stress can exacerbate those symptoms and trigger flare ups.”
The clinic follows a “stepped care” model that matches treatment options to the intensity of patient need. Lower-need patients get the least intensive interventions, like help navigating the health care system or self-directed resources. Those struggling with debilitating conditions get the most intensive care, which could include talk therapy and pharmacological management.
Care is regularly reviewed and stepped up or stepped down based on patient need and level of distress.
UHN’s model was adapted from similar set-ups created in the United Kingdom by the National Institute for Health and Care Excellence and King’s College.
“We are meeting the patient where they are,” says Shannon. “Providing the right kind of support at the right time.”

Depending on the severity of symptoms, patients may see a psychiatrist, a nurse practitioner or a social worker, or even all three.
“We saw a clinical need for this type of care and realized for it to be sustainable, we needed an interdisciplinary team and an integrated care model,” says Dr. Tan.
Nicole, the social worker, not only supports patients’ therapy, but connects individuals to seniors’ programs, housing or employment agencies, income replacement programs or navigating disability support or EI sickness benefits.
“There are complex systems that most people are not aware of and would not have been aware of until they had an unfortunate illness come into their lives,” says Nicole.
The MHIM team hopes each referral builds awareness of their existence across UHN, and helps colleagues in medical and surgical care identify patients who might benefit from mental health care.
“Patients shouldn’t be the ones to have to ask for help for their mental health,” says Shannon. “Why is the burden put back on them?
“In every visit their mental health should be assessed, and support offered if needed.”
Next up for the clinic? Incorporating group therapy, developing digital mental health resources, and using patient data to better understand the connections between mental and physical health.
The Mental Health in Medicine Clinic is available to patients currently seen by a UHN program or clinic. Patients seeking mental health care support to optimize their physical health while they receive outpatient care are eligible for up to six months of treatment. Any UHN physician or nurse practitioner can send a referral via Epic. Note that that individuals who are receiving a single-consultation at UHN or those currently receiving psychiatric care, whether at UHN or elsewhere, are not seen in the MHIM. The clinic can be contacted at [email protected].