A UHN-led clinical trial is making important waves in the fight against primary biliary cholangitis (PBC), offering hope to those living with this progressive and often debilitating condition with no known cure.
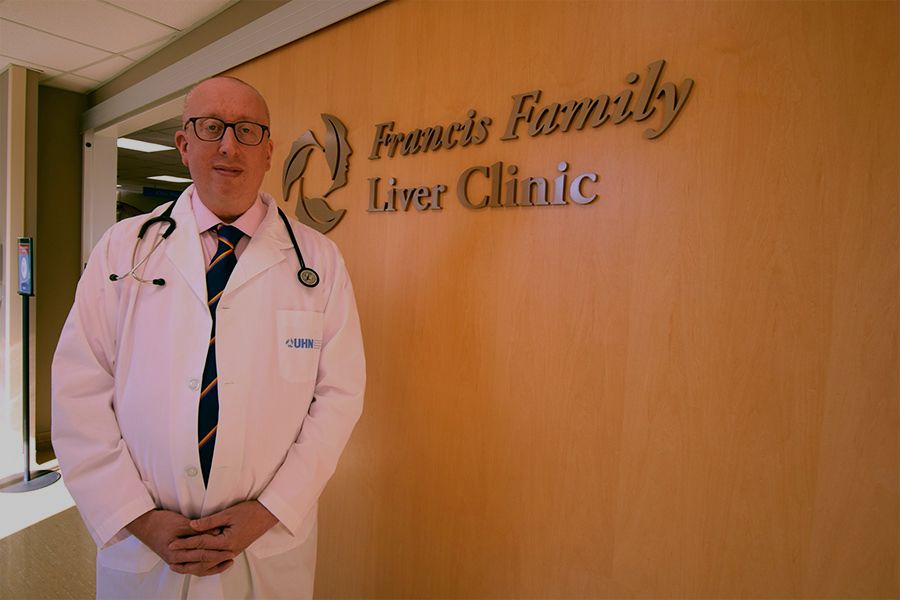
The lead author, Dr. Gideon Hirschfield, is Director of the Autoimmune Liver Disease Program at UHN’s Francis Family Liver Clinic and Toronto Centre for Liver Disease, and holds the Lily and Terry Horner Chair in Autoimmune Liver Disease Research.
PBC, a rare autoimmune disease, wreaks havoc by damaging small bile ducts and causing bile acids to accumulate, leading to inflammation, fibrosis and potentially liver failure. It also can significantly impair patient quality of life.
Toronto General Hospital is home to one of the world’s leading autoimmune liver disease clinics.
Dr. Hirschfield, who is also a principal investigator at UHN’s Schwartz Reisman Liver Research Centre and a clinician scientist at Toronto General Hospital Research Institute, was the lead author of this phase 3 international clinical trial that investigated the potential of a new drug, called seladelpar, developed by CymaBay Therapeutics, as a new potential option for PBC treatment.
The article was published in the New England Journal of Medicine on February 21, 2024, and has received world-wide attention due to the impressive results.
One of the common and debilitating symptoms of PBC is pruritus, or severe itching. More than itching as if from a rash, sufferers describe it has a feeling under the skin, or like having insects crawling on you.
A key welcome result of the clinical trial was not only the impact on liver tests for participants, but also a high number of participants receiving the new therapy reported a notable decrease in the itching sensation, bringing better quality of life.
‘Exciting news that gives new hope to PBC patients’
Currently, there are only two other approved drug therapies available to PBC patients, and one of them can at times make the itching worse. Nearly 40 per cent of patients do not fully respond to treatment, and these patients are seeking treatments that improve the disease and their quality of life.
Patients with PBC can face a lifelong struggle as their disease continues to progress with devastating effects on their quality of life. If PBC progresses too far, liver transplant is the only option for extending life.
“A new treatment option that can slow the progression of PBC, reduce the need for liver transplantation and also improve quality of life by mitigating PBC itch is exciting news that gives new hope to PBC patients,” says Gail Wright, who was diagnosed with PBC in 2012 and is President of the Canadian PBC Society.
Dr. Hirschfield agrees, adding, “this new treatment marks a pivotal moment in the fight against PBC.”
“Not only does it offer hope where options were once limited, but its safety and effectiveness over the course of the 12-month study bring newfound reassurance to patients and providers alike,” Dr. Hirschfield says. “It’s a really exciting time for patients with hope that seladelpar will soon become a new approved drug for patients.”
There is a long and distinguished history of treating PBC at UHN. In 1994, Dr. Jenny Heathcote, founder of the Francis Family Liver Clinic, worked on developing the first therapeutic option, which still works for many patients today.
In 2009, Dr. Hirschfield and colleagues described the gene variants associated with developing the disease, and in 2016 he also contributed to reporting the results of a therapy called obeticholic acid, which is used as a second line agent.
This new exciting work has potential for giving more choice for PBC therapies in the near future.
“Research and medicine are about building on the work and discoveries that came before,” Dr. Hirschfield says. “It is genuinely wonderful to help carry on the tradition of finding new ways of slowing the progression of PBC and giving patients better quality of life.”
Dr. Gideon Hirschfield’s research program is generously supported by donors to UHN Foundation.

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.