Dr. Gelareh Zadeh is a pioneer in the field of brain cancer research and neurosurgery. (Photo: Regina Garcia)
A brain cancer diagnosis can be devastating for the thousands of Canadians who receive one each year.
It’s historically been difficult to treat, and only 21 per cent of patients with brain cancer survive beyond five years.
Dr. Gelareh Zadeh, one of the world’s most sought-after neurosurgeons and researchers, knows these statistics too well. She’s seen too many patients suffer from brain cancer, which is why she’s made it her mission to bring the most cutting-edge, modern and innovative technologies and treatments to UHN’s Krembil Brain Institute (KBI).
In 2019, Dr. Zadeh, Medical Director of the KBI, Dan Family Chair in Neurosurgery, Wilkins Family Chair in Neurosurgical Brain Tumour Research and Head of the Division of Neurosurgery in the Sprott Department of Surgery at UHN, brought in the latest addition to the KBI’s brain cancer-fighting arsenal: a laser interstitial thermal therapy (LITT) system, made possible through the generous donation of a grateful patient.
With this state-of-the-art laser technology, clinicians no longer have to surgically operate to reach a tumour or lesion.
“You convert an open operation that has multiple days of admission, need for recovery and exposure of normal brain tissue into a minimally-invasive procedure,” explains Dr. Zadeh, adding that patients recover much more quickly and are at less risk than they would be with traditional open-skull brain surgery.
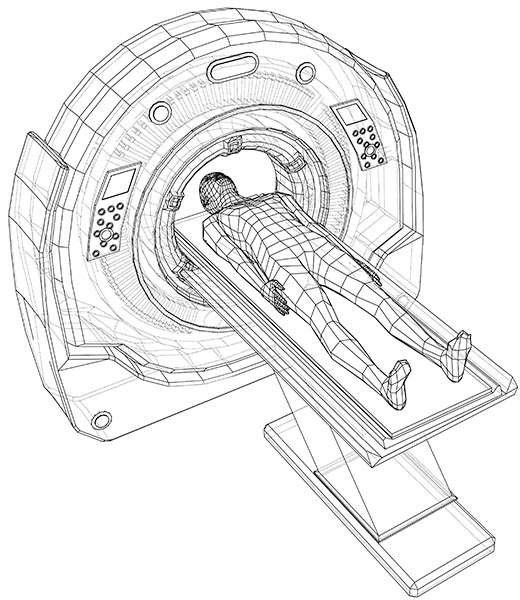
With LITT, surgeons insert a pen-sized probe through the skull. Once the probe is inside the brain, a laser heats the diseased tissue and liquefies it, allowing it to be removed with a suction. The patient lies in an MRI machine throughout the operation so surgeons can image their brain in real-time.
The true game-changer? The LITT can access previously inoperable tumours and lesions in patients with epilepsy, as well as brain cancer.
“We used to just manage these hard-to-access tumours medically and symptomatically,” says Dr. Zadeh. “Now we can get rid of them.”
Decades of innovation
Dr. Zadeh sought out this technology – the KBI is one of two centres in the country that can do this procedure – because it’s critical to her that the KBI remain at the forefront of neuro-oncology.
Nearly 20 years ago, the KBI began using Gamma Knife, which, at the time, was a groundbreaking technology that continues to save patient lives today. It works by sending focused beams of radiation to precise areas of the brain.
While Gamma Knife is still a critical tool, LITT allows Dr. Zadeh and her colleagues to get at even more complicated cancers.
“This is an incredibly innovative technology. I wanted to acquire it so we could continue to stay at the cutting edge,” she says, adding that the expertise of two of her colleagues, Dr. Suneil Kalia, who has a functional neurosurgery background, and Dr. Paul Kongkham, who has extensive oncological knowledge, has been instrumental in getting the technology up and running safely.
Dr. Zadeh is also pushing brain cancer boundaries in her lab. Together with scientist and collaborator Dr. Daniel De Carvalho, she has developed a groundbreaking blood test that can detect not only whether someone has brain cancer but the specific type of brain tumour, too.
This has tremendous implications for patients.
“It’s potentially a replacement for the need to do a biopsy diagnosis,” says Dr. Zadeh. “Ultimately, we hope it could be used as a tool for early detection of brain cancer and to assess response to therapy and detect recurrence early.”
Dr. Zadeh and her team published a paper on the blood test in May 2020 and are now conducting trials to see if it can become a clinical-grade test.
Dr. Zadeh says that in addition to Ontarians, she and her team would welcome an opportunity to care for out-of-province patients using the LITT technology and will work with patients and their healthcare teams to make this happen.
“It’s a technology at the intersection of neuroscience and cancer,” she says. “It gives us the advantage of bringing the two worlds together.”
Read more in the Krembil Brain Institute magazine.


