Melissa Ramrup was able to have a baby despite an endometrial cancer diagnosis, thanks to the team at UHN. (Photo: Tim Fraser)
By Elizabeth Chorney-Booth
By March 2020, Melissa Ramrup had finally reached the point in her life when she felt ready to have children. The now 41-year-old from Markham, Ont., had always experienced irregular periods, but at the time, some unusual bleeding led to a scan that revealed polyps on her uterus, which were soon diagnosed as endometrial cancer. Suddenly, her dream of a family was in jeopardy, as she faced the frightening prospect of undergoing treatment for gynecological cancer. Early endometrial cancer generally has a good prognosis, but the standard treatment is a hysterectomy, which would leave Ramrup unable to become pregnant.

“At first I wanted to go ahead and have the hysterectomy right away,” Ramrup says, admitting that she was worried about losing her life. “I didn’t want to have the cancer in me, and thought I’d just have to give up the idea of ever having a baby myself.”
As it turns out, thanks to a clinical trial facilitated by Dr. Sarah Ferguson, a gynecologic oncologist at University Health Network (UHN), Ramrup would have the best of both worlds. Today, two years after her diagnosis, she is cancer-free and finally a mother.
Dr. Ferguson is working on a clinical study to delay hysterectomies in patients with endometrial cancer by placing a progestin intrauterine device (IUD) to correct a hormone imbalance that often causes the cancer. Normally, the treatment is followed by a hysterectomy at some point, but a small window of opportunity is available for patients like Ramrup to become pregnant, typically through IVF. Dr. Ferguson’s research has shown that the procedure is about 60 per cent successful in reducing cancerous growths long enough for endometrial cancer patients to have children. She was looking for a solution for some of the other 40 to 45 per cent of patients who wanted to safely attempt a pregnancy after their cancer diagnoses, particularly those with an elevated BMI.
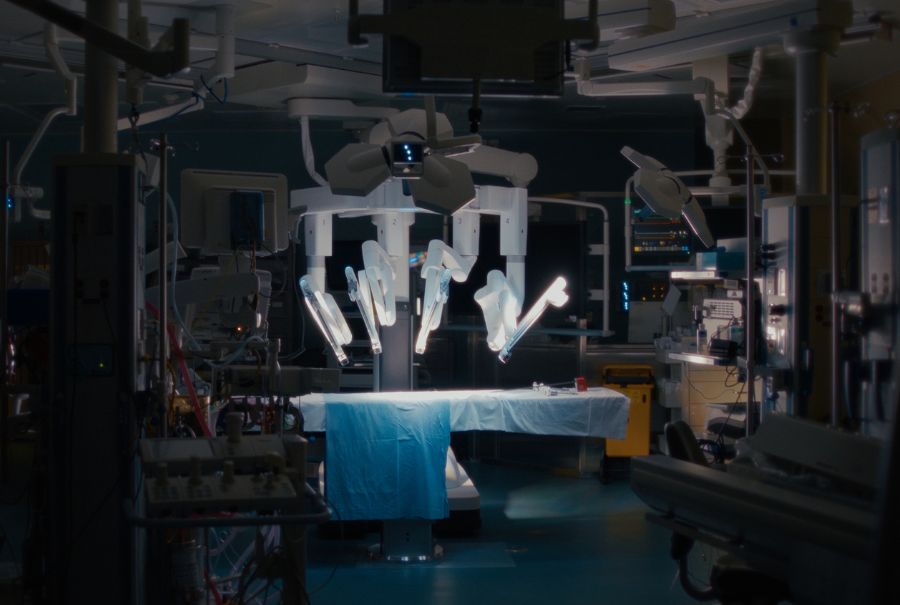
Together with Dr. Tim Jackson, Medical Director of the Operating Room at Toronto Western Hospital, who also leads the Bariatric Surgery Program in the Sprott Department of Surgery and holds the Medtronic Chair in Minimally Invasive Surgery, Dr. Ferguson came up with an idea that could be revolutionary.
– Source: UHN500
Number of bariatric surgeries performed by Sprott Surgery annually.
A new use for a tried-and-true surgery
While obesity can be a contributing factor to various cancers and other diseases, the correlation between endometrial cancer and an elevated BMI is much more direct. Extra weight can trigger metabolic abnormalities that affect hormone balance and allow endometrial growths to develop. Dr. Ferguson knew her colleagues in the Sprott Department of Surgery perform bariatric surgery – particularly sleeve gastrectomies, which significantly reduce the size of a patient’s stomach, thus limiting caloric intake and resulting in relatively quick weight loss – as a preventive measure against obesity-related diseases. She wondered if bariatric surgery to prompt quick and significant weight loss could help combat endometrial cancer, allowing patients of child-bearing age to delay and even avoid hysterectomies. The hope is that the surgery and subsequent weight loss will act to change patients’ metabolic state and naturally balance hormones in a more effective and permanent way than a progestin IUD could on its own.

Dr. Ferguson to treat endometrial cancer patients in a new way. (Photo: Tim Fraser)
“Regular monthly periods offer the protection of progestin to help balance estrogen, but patients with a higher BMI don’t always ovulate every month, so their uterine lining can grow and cause cancerous changes,” Dr. Ferguson says. “If losing body mass and changing a metabolic state prevents endometrial cancer in all age groups, as studies have shown over and over, can we use bariatric surgery to treat cancer by lowering body weight?”
Surgical collaborations
Sprott Surgery just happens to have a world-class Bariatric Surgery Program, one of the oldest and most robust in the country. As an elective procedure, bariatric surgery is not usually performed on cancer patients, since the disease and traditional therapies like chemotherapy can create a heightened risk, but Drs. Ferguson and Jackson came up with a plan to not only operate on endometrial cancer patients with a BMI of at least 35 (patients approved for bariatric surgery typically have a BMI of 40 or above unless there are other immediate health concerns), but also expedite the process so they can reap the benefits before their cancer progresses. In 2022, together with their team, Drs. Ferguson and Jackson initiated a small randomized trial, implanting some of her patients with just the IUDs and offering others the IUDs along with sleeve gastrectomy surgeries.
“With the IUDs, it felt like I was trying to change cancer outcomes, but I hadn’t changed what was driving the cancer in the first place,” Dr. Ferguson explains. “Researchers are now looking at cancer risk and treatment in a much more holistic way. We’re trying to use surgery to help treat a cancer in a way that isn’t just removing it but trying to treat the pathways that are driving it.”
Bariatric surgery is often misunderstood and carries a certain degree of stigma – despite the surgery’s track record of preventing disease and changing patients’ lives, there is still a cultural misperception that the procedure is little more than a quick fix to replace a healthy diet and exercise regimen. The UHN trial is currently not designed to prove the surgery has positive outcomes when it comes to either fertility or cancer (though they are certainly keeping track of those measures) – it’s trying to determine if patients are even willing to consider bariatric surgeries in place of hysterectomies. Only a handful of patients have participated in the trial so far, but Dr. Jackson says he’s excited to apply this surgery that has changed the lives of so many patients to a new cohort.
“It’s a totally different way of thinking about treating this cancer,” Dr. Jackson notes. “It’s such a nice way of doing it because not only do we actually treat the disease, but also we treat the overall health of the patient. Then the third bonus is really that we don’t burn bridges for fertility and family planning. It really is a triple win.”
– Source: Canadian Cancer Society8,100
Estimated number of Canadian women diagnosed with uterine cancer in 2022.
Dealing with different kinds of patients

Dr. Jackson says his more traditional bariatric surgery patients are often surprised to learn how safe and non-invasive the procedure has become over the years, with patients usually being discharged the day after their operation. That said, the complicated part of the procedure is the pre-surgery intake process, as well as the aftercare – the sleeve gastrectomy is not a magic bullet, and patients need to be prepared to be active participants in their weight loss. Katie Warwick is a patient care coordinator and registered dietitian in the Bariatric Surgery Program in the Sprott Department of Surgery. Typically, she and her team will spend up to one year consulting with prospective patients to ensure they’re good candidates for the surgery, are psychologically and medically fit, and can commit to one year of followup care. The process is expedited to about four months with Dr. Ferguson’s patients to address the urgency of the cancer.
“Our usual patients need to pass through an assessment pathway in order to qualify for surgery,” Warwick says. “But for these expedited cases, it’s more of a preparation pathway. We’re preparing them for the surgery and putting more of the focus on the education piece to make sure they feel ready and have the knowledge they need to be successful.”
The trial is still in the early stages of assessing if the bariatric surgery route is even feasible, but Dr. Ferguson says she’s seen early successes, and some of the first patients who have tried the surgery are now cancer-free and undergoing IVF treatment to attempt pregnancy. Both Drs. Ferguson and Jackson are hopeful their collaboration will result in a full clinic, helping patients with elevated BMIs have the same joy Ramrup has experienced in realizing her dream of pregnancy even after an endometrial cancer diagnosis.
“These treatments are about saving a life, but I’ve also been given the opportunity to have a child, which is very emotional,” Ramrup says. “I’m very thankful to be part of this journey that the doctors have put so much work and dedication into. They’ve given us so much hope.”