The Canadian Concussion Centre at Toronto Western Hospital, UHN, stands as one of Canada’s leading institutions dedicated to concussion research and treatment.
Overseen by internationally acclaimed neurosurgeon Dr. Charles Tator and neurologist Dr. Carmela Tartaglia, this world-leading centre treats more than 1,200 patients annually and houses Canada’s only dedicated Concussion Fellowship Program.
As we mark Concussion Awareness Week (September 21-27), the Canadian Concussion Centre’s team of world leaders in imaging, genetics, neuropsychology, and psychiatry continues advancing our understanding of this critical health issue that affects hundreds of thousands of Canadians each year.
Below, Dr. Charles Tator shares his insights on this complex medical condition.
How do you define concussion?
A concussion is a brain injury with potentially devastating results. The dilemma is that we don’t really understand its biology. We can’t pinpoint the exact brain sites that cause concussion or identify damage on CT scans or MRIs – and despite advanced imaging technologies, there’s no physiological or biomarker test for concussion.
Concussion is caused by direct or indirect force that makes the brain accelerate within the skull. It is likely a “jiggle” of the brain – especially rotational movement, but also linear acceleration. When your head turns from a punch or hitting the ice for example, that rotatory movement can produce the angular acceleration (rapid rotational motion) or linear acceleration that results in concussion. The brain moves within the skull because it’s surrounded by spinal fluid.
What are the symptoms of a concussion?
There are about 65 different possible symptoms, not all present at once. These include headaches, nausea, vomiting, personality changes, or memory problems.
Symptoms also evolve over time – someone might have one symptom at first, others might have 10 or become dizzy later when they weren’t initially.
You could have a concussion even without passing out. Symptoms can take hours or days to develop. Most people recover in 10 days to four weeks, but many take much longer and some people never recover.
How common is concussion?
There are 400,000 concussions annually in Canada. In 2022 alone, 573,000 Canadians aged 12 and older reported concussions. Children under five and women over 65 have the highest rates.
Alarmingly, pediatric concussion visits have quadrupled in Ontario since 2010, and many concussions go unreported, especially in sports where there’s pressure to continue playing, making the true numbers likely much higher.
What causes concussion?
While falls are the most common cause across all ages, concussions can result from car crashes, sports injuries, workplace incidents, intimate partner violence and even home accidents. In fact, household accidents account for one in seven concussions.
The key factor is linear or rotational brain movement. It’s not necessarily about hard hits – even minor impacts can cause the brain to jiggle inside the skull, disrupting normal function.
Can you speak to the dangers of “second-impact syndrome”?
This is when someone gets a second head injury before fully recovering from the first. Though rare, it’s often deadly. You can get terrible brain swelling and dangerous pressure increases that occur rapidly and may be impossible to control.
Second-impact syndrome affects primarily young male athletes aged 13 to 24, with 95% of cases in children under 18. The mortality rate is over 50%, with nearly 100% permanent disability rates.

How can we prevent concussions?
We have discovered some treatments for only some of the symptoms of concussions, so prevention is crucial. In hockey, we need to ban all hits to the head, eliminate fighting, and get rid of deliberate elbows and shoulder impacts to helmeted heads.
But here’s a critical myth: helmets don’t prevent concussions. They’re like another skull on top of the skull, but virtually all kids playing hockey are wearing helmets when they get concussed. They may be able to prevent skull fractures and some more damaging head injuries, but helmets can’t stop the brain from moving inside during impact and therefore cannot prevent concussions.
Home safety is equally important – remember, household chores account for one in seven concussions. Remove tripping hazards, ensure good lighting throughout your home, install safety gates for stairs, and use window stops. For children, supervise them constantly and childproof your environment. Falls are the leading cause of concussion in older adults, so handrails, non-slip mats, and clearing walkways are essential. Canes and walkers can be lifesaving!
Education and rule changes work. Hockey Canada’s ban on body checking for 11- to 12-year-olds resulted in a 70% reduction in concussion risk – about 4,800 fewer concussions across Canada. Let’s increase the age for bodychecking in hockey to 18.
Ontario is the only province with a concussion law. Can you tell us about Rowan’s Law?
Rowan Stringer was a 17-year-old rugby captain who died in 2013 from second-impact syndrome after playing three times in six days, during which she sustained concussions. Her tragic death led to Canada’s first concussion legislation in 2018.
Now, Rowan’s Law requires sports organizations to ensure athletes, parents, coaches, and officials review concussion awareness resources annually. It mandates concussion codes of conduct and removal/return-to-sport protocols. Ontario is leading the world in concussion safety legislation – and we hope the rest of Canada and the world will follow.
When should someone seek help?
If you think you have a concussion, stop what you’re doing and seek medical help immediately. If someone’s unconscious, call 911.
In Ontario, only doctors and nurse practitioners can medically diagnose concussions, and other provinces allow other health care professionals to make the diagnosis. Don’t wait – even mild symptoms warrant medical attention since symptoms can take hours or days to develop.
How is concussion treated?
The frustration is that we have nothing that eliminates symptoms completely. Current concussion management includes relative cognitive and physical rest for the first day, then a gradual return to activities. Today, we stress early return to physical activity, but complete avoidance of activities that may cause another concussion until medical clearance has been obtained.
Recovery varies enormously – anywhere from a week to a year or never, depending on the individual. The fastest someone should return to sports activities is about two weeks, but it could take much longer.
What services does UHN offer for concussion patients?
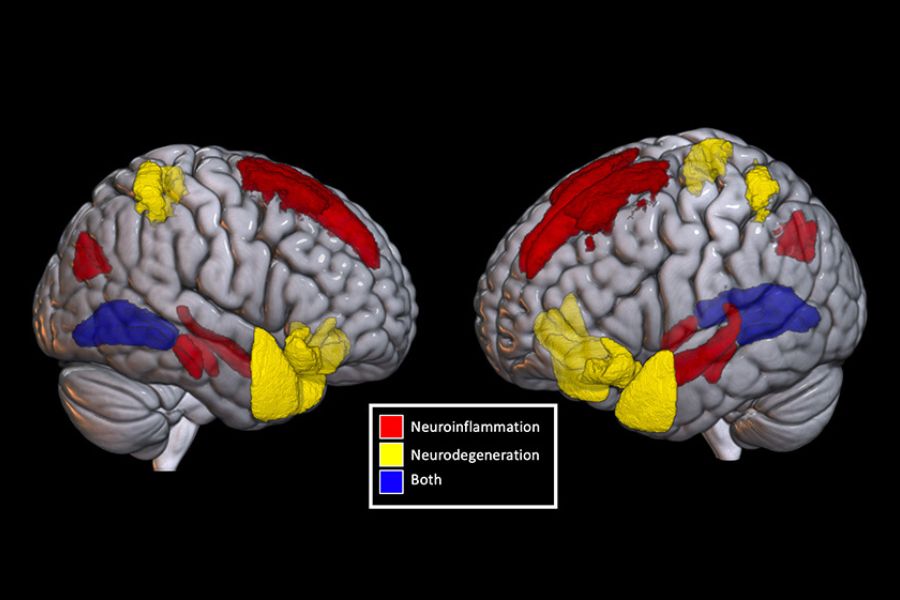
UHN’s Canadian Concussion Centre serves the 30% of concussion patients who don’t fully recover and experience persisting symptoms. We use artificial intelligence (AI), advanced imaging (MRI, MEG, PET), eye movement tracking, blood biomarkers, and neuropsychological testing.
We’re researching chronic traumatic encephalopathy (CTE) in living patients, and have Canada’s only brain donation program targeting retired athletes with repetitive concussions. We are also focused on reducing wait times while advancing research.
A progressive neurodegenerative disease associated with repeated traumatic brain injuries, CTE typically develops years or decades after the initial brain trauma, with symptoms often appearing in middle age or later.
Can you speak to some exciting research developments in concussion research?
A big mystery is why some players with dozens of concussions don’t develop CTE while others do. We’ve definitively shown that repetitive concussions cause CTE in some hockey players, but individual variation is enormous – that is a key research frontier. We are also developing imaging techniques to detect CTE in living patients and investigating biomarkers for earlier diagnosis.
Finally, our work with Ontario’s government has shown that increased concussion awareness initially increased clinic visits, then decreased them over time due to better prevention. This proves research can directly improve outcomes and save lives.
We have also been determining ways to assess concussion in workers and develop improved assessments and processes for aiding return to work after concussion.
Moving forward
The Canadian Concussion Centre continues to lead global concussion research, driving our mission to prevent tragedies like Rowan’s while serving thousands of Canadians living with concussion effects daily. Through continued research, education, and prevention efforts, we work together to reduce the devastating impact of concussions on individuals, families, and communities across Canada.
For more information, including our outstanding webinar series held every two weeks, please visit the Canadian Concussion Centre site here.

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.