
KITE post-doctoral fellow is reimagining patient sleep-monitoring technology with wearable tech
Dr. Ivana Culjak, a post-doctoral fellow at Toronto Rehab is developing a wearable system to detect a build-up of fluid in patients’ lungs while they sleep. Indicative of heart failure, this symptom could result in further life-threatening complications and require hospitalization. Dr. Culjak is currently completing her work at KITE (Knowledge Innovation Talent Everywhere), one of the principal research enterprises at UHN and a world leader in complex rehabilitation.
Heart failure affects more than one million Canadians, with 50,000 new patients diagnosed every year.
The progression of heart failure towards hospitalization is initiated by an occurrence known as a “lung water cascade”. Patients will first experience elevated blood pressure in the lungs, leading to a build-up of fluid, which then results in clinical symptoms such as dyspnea – an intense shortness of breath likened to a feeling of suffocation.

Past fluid monitoring systems could only be used in the lab as they required external electrodes to detect signals and a technician had to be present to press a button every 3-5 minutes. In addition to the circuit board, Dr. Culjak’s prototype includes a conductive, shirt-like garment which would replace the external electrodes and could be worn for up to 24 hours. The device would be able to send the patient’s data to sleep experts remotely – allowing the patient to remain at home while being observed by their health care provider.
By proactively monitoring patients and analyzing changes in their bodies before symptoms appear, there will be more time for intervention and changes in treatment, keeping patients out of hospitals. In 2023, Transform HF – a joint partnership between the University of Toronto and the Ted Rogers Centre for Heart Research to transform the lives of heart failure patients – awarded Dr. Culjak with a Trainee Award for her work on this project.
“A major challenge of current remote monitoring technologies for patients with heart failure is that they have not been co-designed with patients, taking into account their social, cultural or local context,” says Dr. Culjak. “This project aims to use a person-centered textile-based solution for convenient, accessible and at-home monitoring, with the potential to improve health outcomes and quality of life.”
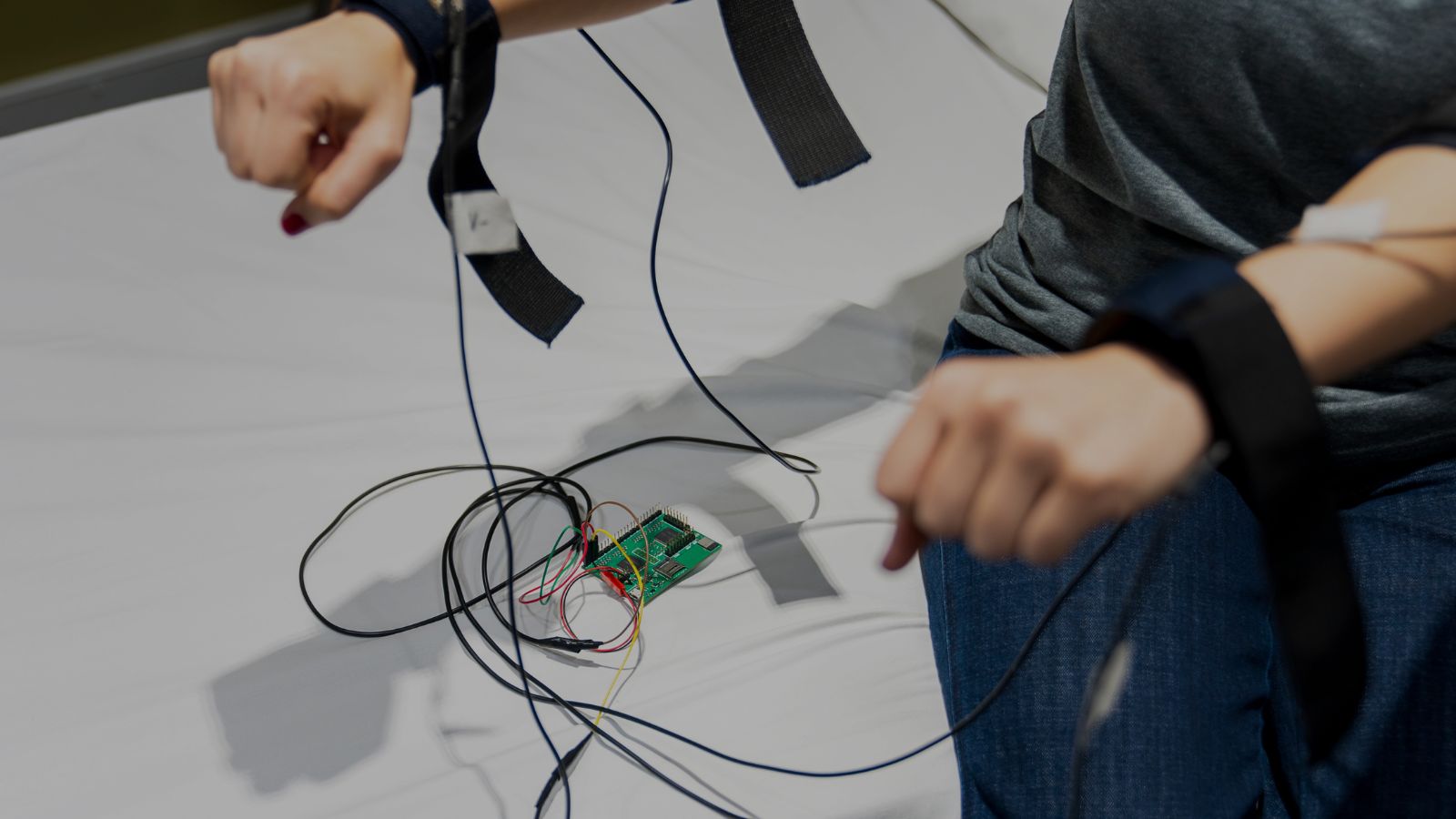
An electrical engineer by training, Dr. Culjak collaborated with many other experts – biomedical engineers, material and textile engineers, cardiologists and graduate students – to produce this first prototype. After all, no one ever changed the world on their own.
Dr. Culjak is now working on the second prototype at KITE’s SleepdB lab, one of the few laboratories in the world dedicated to understanding the intricate interplay between sleep, body fluid shifts and respiratory disease. Once she has completed the second prototype, she will seek approval to use this device on patients, at which point she will be able to run clinical trials and secure a patent. With her fellowship concluding at the end of April, Dr. Culjak hopes to continue her work at UHN on this project.
“Heart failure affects over a million Canadians, making it a significant health issue,” says Dr. Culjak. “Supporting this research is important for the Canadian community.”

No one ever changed the world on their own but when the bright minds at UHN work together with donors we can redefine the world of health care together.


