Blood samples provide the information needed for Dr. Kathryn Howe’s research. She wants to know whether certain biomarkers can predict more severe cases of COVID-19.
By Claire Gagné
The Peter Munk Cardiac Centre is known for its ingenuity and world-leading research. The COVID-19 pandemic has put this reputation to the test and highlighted the Centre’s leadership in the field. The need to pivot instantaneously has been unprecedented, but if there’s any group that can rise to the challenge, it’s the team at the Peter Munk Cardiac Centre. Physicians, nurses, allied health providers, technicians – everyone has come together to solve problems they could have never imagined. What they have been learning since those early days of the pandemic will help shape the future of care far beyond it.
Questioning the root cause of COVID-19
In the spring of 2020, Dr. Kathryn Howe, a vascular surgeon and scientist in the Peter Munk Cardiac Centre at UHN’s Sprott Department of Surgery, wanted to figure out what caused this disease to affect an individual’s heart. COVID-19 was known as a respiratory disease, but was there more to it? Dr. Howe was trying to make sense of early reports from vascular surgery colleagues in the United States of unusual blood clots in the veins and arteries of patients with COVID-19. “I started bringing that to the team in the lab and saying, ‘look, we’ve got to talk about this,’” she recalls.
Dr. Howe and her mentor, scientist Dr. Jason Fish, collaborated to write a review paper suggesting the endothelium, cells that line every blood vessel in the body, might be the linchpin in patients infected with the novel coronavirus. They realized the special protein that exists on COVID-19 is what might allow it to bind to the endothelium and potentially put those cells at risk. Many of the complications we’re now familiar with, such as COVID toes (the dark spots on toes caused by small blood clots), as well as peculiar strokes in otherwise healthy people and neurological effects like loss of smell or taste, relate to the vascular system. “These cells line every single system,” Dr. Howe says. “There’s almost no place where they are not being impacted by the virus.”
Dr. Howe is now working with colleagues in radiology and cardiology – Dr. Kate Hanneman and Dr. Dinesh Thavendiranathan, respectively – on a study that’s testing endothelial cell dysfunction in blood samples from patients with COVID-19 to see if there are any signs that might predict more severe cases of COVID-19-related cardiovascular disease. With followup imaging, they are also exploring whether the infection has made any subtle changes to the heart that might precipitate longer-term effects.

Using virtual care to help patients at home
Meanwhile, Dr. Yas Moayedi, a heart failure cardiologist at the Peter Munk Cardiac Centre and researcher at the Ted Rogers Centre for Heart Research, had a practical problem to solve: How do you provide care for patients with COVID-19, some of whom are very ill but not sick enough to be admitted to the hospital during a pandemic? You create a COVID-19 virtual care clinic to remotely monitor patients. “We had to do something that had never been done before and in record time. It was a herculean effort,” she says.
Within two weeks, the COVID-19 Virtual Clinic was up and running across University Health Network (UHN), involving a large multidisciplinary team – 47 clinicians from 11 different specialties. There is a “circle of care,” in which patients are seen virtually by any subspecialist, given the uncertainties associated with the virus. The COVID-19 Virtual Clinic has helped reduce admissions to UHN’s Emergency Departments for stable patients. Through an interdisciplinary team of specialists, it has ensured deteriorating patients are identified quickly for appropriate treatment.
The Clinic, which had seen more than 9,000 patients by last November, has proven how effective remote monitoring can be. Based on what Dr. Moayedi and her team have learned, virtual care across disciplines will be here to stay in a patient-centred model.

A device for the most critically ill
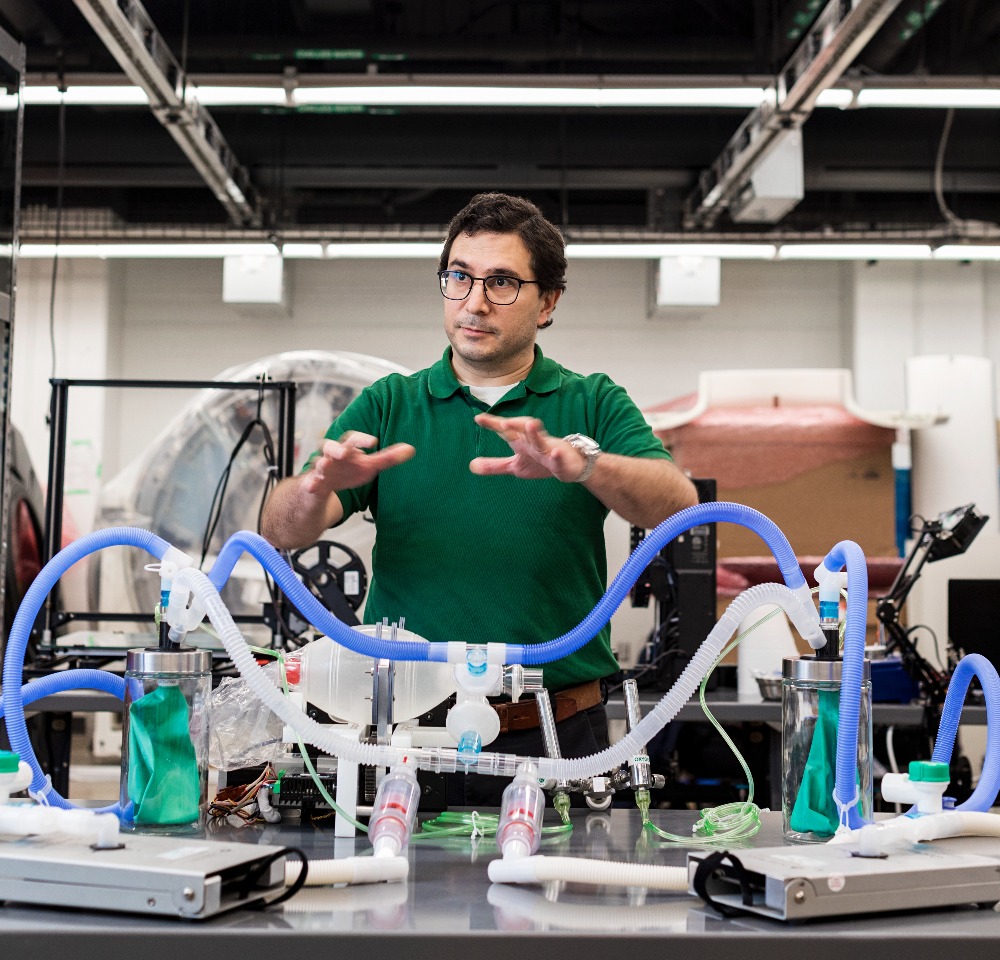
One early challenge for hospitals was securing enough ventilators to help patients with COVID-19 in intensive care units. While governments began buying ventilators, Dr. Azad Mashari, an anesthesiologist at the Peter Munk Cardiac Centre and Toronto General Hospital’s Department of Anesthesia and Pain Management, had an idea. Three decades earlier, a colleague, Dr. Joe Fisher, had devised a way to use a primary ventilator to support more than one patient – otherwise known as a “split ventilator.”
Dr. Fisher’s initial results were published in a medical journal but had gone largely untouched – until there arose a sudden need to ventilate a large number of people at once. Dr. Mashari and his team set out to make Dr. Fisher’s design field-ready and manufacture a safe and more effective option for ventilator splitting. This would be a last resort backup system in case standard ventilator supplies were exhausted.
More than a hundred people from numerous departments worked in the Lynn and Arnold Irwin Advanced Perioperative Imaging Lab at the Peter Munk Cardiac Centre to build a prototype, using and modifying standard medical parts and locally manufacturing components. “It was a mass collaboration effort,” says Dr. Mashari.
For many countries, ventilator shortages continue to pose a constant risk to patients. Dr. Mashari and his team are sharing their design and test results, and have published an account of what they learned so colleagues around the world can have the support they need when in crisis.
With the demands of COVID-19 evolving, having in-house experts who can innovate at a moment’s notice means physicians can continue to provide world-class care in any situation.
This article originally appeared in the 2021 Peter Munk Cardiac Centre annual report. Read it here.
Photos by Tim Fraser.


