Joselito Abaday, a Patient Care Coordinator in the Cardiovascular Intensive Care Unit at the Peter Munk Cardiac Centre, is pictured here with an iPad and a makeshift stand which allows patients to see their loved ones without having to hold the device. (Photo: UHN)
For the past three weeks, Brenda Sears-Anderson has joined her 80-year-old mother for dinner every night at 6 p.m. But they aren’t physically together – Brenda’s mother was hospitalized at Toronto Western Hospital (TWH) last month with COVID-19.
They’ve been connecting through video, using donated iPads, tablets and phones that have been deployed across UHN inpatient units.
In March, hospitals across Ontario were instructed to restrict visitors. UHN had to adjust quickly to keep patients and staff safe from the spread of COVID-19. Barring a few exceptional circumstances, patients are not be able to physically have their loved ones with them in the hospital.
At UHN, families are an essential part of patient care and support. For Laura Williams, Director of Patient Engagement, and David Wiljer, Executive Director, Education Technology Innovation, it was important to ensure a line of connection between patients and their loved ones was not lost.
“We knew this would be a difficult time for our patients and families,” says David.”From a UHN Digital perspective, our goal is to connect people – and what better way to help than to virtually connect a family member and a loved one?”

Brenda’s mother, who was diagnosed with COVID-19 in April, has been connecting via FaceTime with her daughter every night via an iPad provided by the unit. “Those iPads have been a godsend,” says Brenda. (Photo: Courtesy Brenda Sears)
Thanks to a generous donation from UHN’s three foundations (Toronto General & Western Hospital Foundation, Princess Margaret Cancer Foundation and Toronto Rehab Institute Foundation), that connection was made possible through 125 iPads and tablets for patients to video call with their families and friends.
“Those iPads have been a godsend,” says Brenda, who is also a member of UHN Digital. Her mother, who suffers from dementia, had been transferred to TWH from a long-term care facility when she was diagnosed with COVID-19.
“When we first video called, I hadn’t seen my mother in four weeks – it was so encouraging to hear her voice and see her face,” Brenda says.
The first batch of devices arrived at the beginning of April, and dedicated UHN Digital and Patient Experience teams worked tirelessly to set them up for staff and patients – including developing cleaning protocols, writing scripts and information sheets, and deciding how to best deploy and support the devices across UHN.
“I got to hear from someone whose mother unexpectedly ended up in the hospital,” says Mahvish Malik, Project Manager for the Digital Patient Experience Program. “The relief they had in being able to connect with their loved one reminded me of the impact we have on people’s lives – it was nice to see that unfold in real time.”
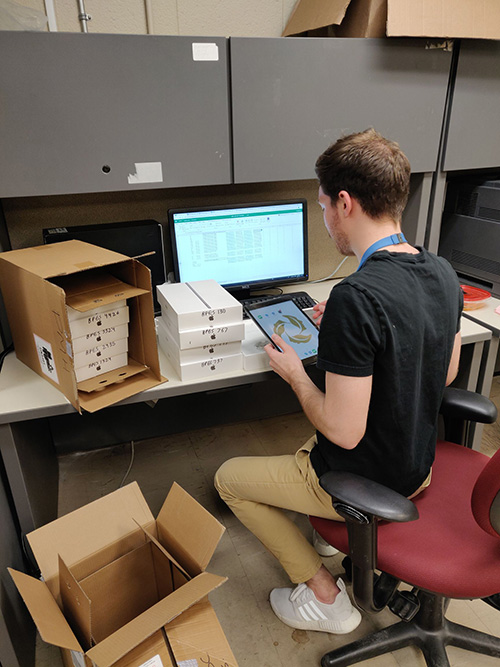
Nicholas Hope, Senior Project Analyst on the UHN Digital team, is programming communication applications on iPads ahead of deployment to inpatient units. (Photo: UHN)
The coordinated efforts of both teams allowed the devices to be deployed before the Easter long weekend, while still considering all facets of patient, frontline staff and technology parameters.
Members of each team, such as Brian Lofgren, Manager and Architect of Endpoint Engineering of Digital Operations, “couldn’t imagine being isolated without any means to communicate with those important to me.”
Putting themselves in the patient’s shoes, they knew how important it was to act quickly.
“There was a big push across the board to get the devices up and running – it was wonderful to witness this kind and compassionate TeamUHN effort,” says Laura. “Being able to see your loved one in hospital is very different than hearing them on the phone.
“For some, their loved ones are very sick, and they aren’t able to travel from out of town to visit – with the help of clinicians, the iPad gave them an opportunity to experience this final goodbye.”
Before deploying the devices, the teams needed to establish measures to reduce the possibility of transmission of infection. Working with UHN’S Infection Prevention and Control (IPAC) team, approved cases were purchased for the iPad as well as an Electroclave, a system which electronically disinfects the devices.
Taking lead from other hospitals, a “Ziploc solution” was also created – once the video call is connected, the device is placed into a Ziploc bag. When the call is finished, the tablet is wiped down, and the bag is disposed of.
“It’s something we gave a tremendous amount of thought to,” says David. “We knew how much these devices were needed, but it wasn’t something we could implement if the right protocols weren’t in place to protect staff and patients.”
Since the devices have been deployed, feedback has been overwhelmingly positive. Staff have noted that patients are feeling less isolated, and video calls have even expanded outside patients with families, with sessions such as music therapy taking place virtually.
“I was involved with the project from the very beginning,” says Valeria Raivich, Manager of Patient Learning and Experience Centres. “I saw firsthand just how committed our teams are to providing patients, families, and staff with communication support to ensure our patients have the best patient experience possible under the circumstances.”
For Brenda, being able to see her mother has alleviated a lot of anxiety. Being her primary caregiver, Brenda knows the right questions to ask to make sure her mother is comfortable and feeling OK – and it takes seeing her facial expressions to sometimes know her real answer.
“I can really tell how she is and her well-being by physically looking at her,” says Brenda. “She’s on the mend now – but I miss her lots and every day that I get to see her face is cherished.”
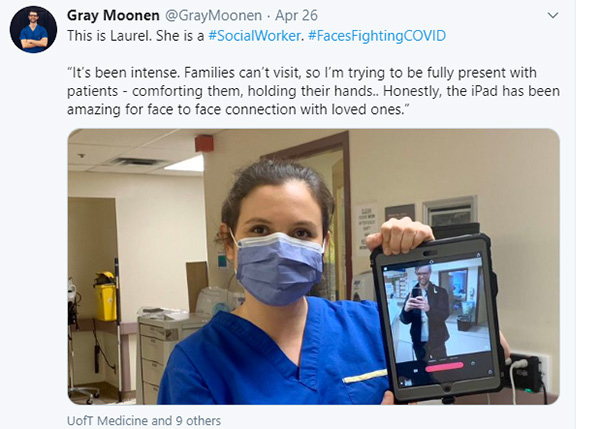
Dr. Gray Moonen, a Family Medicine Resident at UHN, documents a UHN social worker using the iPad as part of his #FacesFightingCOVID series.


