Patients treated within this model, which integrates nursing and psychiatry (INaP) support with an interdisciplinary clinical team, were found to have greater reduction in dizziness-related disability as compared to patients treated by interdisciplinary team only. The results of the evaluation were published recently in The Laryngoscope, a leading publication focused on advances in the diagnosis and treatment of head and neck disorders.
“This innovative model, where psychiatric support is embedded within interdisciplinary patient care from the beginning, while also providing access to a nurse clinician, has greatly contributed to improved outcomes for our patients,” says Dr. Philip Gerretsen, lead author and a clinician-scientist at UHN who studies the intersection of medical conditions with mental health issues. Wanda Dillon, a Clinical Vestibular Nurse at the Hertz Clinic, co-authored the paper, together with several collaborators.
“Patients frequently feel lost, alone and unsupported with debilitating symptoms of dizziness and imbalance, which impair their ability to work, socialize and maintain a reasonable quality of life,” Dr. Gerretsen continues. “This approach attempts to address these inadequacies so patients feel supported and cared for by an available, accessible team that works toward addressing both patients’ physical and mental health needs. Encouragingly, given the scarcity of healthcare resources to treat chronic dizziness, INaP is also able to serve a higher volume of patients than the traditional approach to care.”
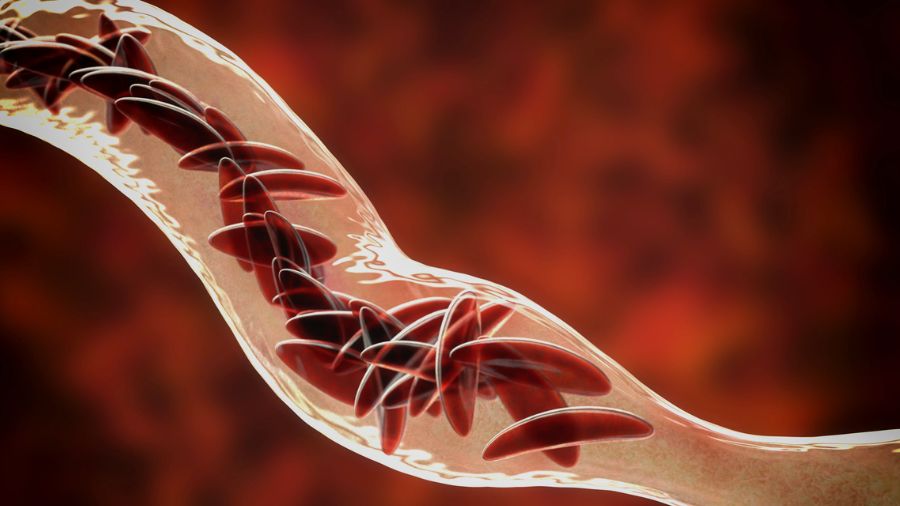
Dizziness and imbalance are among the most common complaints in medicine, affecting approximately 20 per cent to 30 per cent of patients worldwide and contributing to reduced quality of life.
In UHN’s INaP model, an interdisciplinary healthcare team consisting of a neurotologist, neurologist, vestibular physiotherapist, psychiatrist, and nurse clinician together provide an assessment which includes both a neurotological and psychiatric evaluation.
The nurse clinician acts as the hub of care during this process, providing education, treatment guidance, psychotherapeutic support, and care coordination. This support, whether in-person, by phone, email or other electronic platform, helps address the psychosocial and attachment needs of patients and their families/caregivers that can arise due to the patient’s illness.
In most current models of care, dizziness is treated via an “assess and refer” process where a patient is evaluated by one specialist after another with a focus on the vestibular/non-vestibular causes of their condition. Mental health evaluation is left for later consideration, often resulting in persistence of the patient’s dizziness.
“Our research shows that this model better aligns available resources as efficiently as possible to support our patients’ functional recovery,” says Dr. Gerretsen. “As we continue to recognize the role of mental health in many chronic diseases, this is a model to be considered in treating them.”