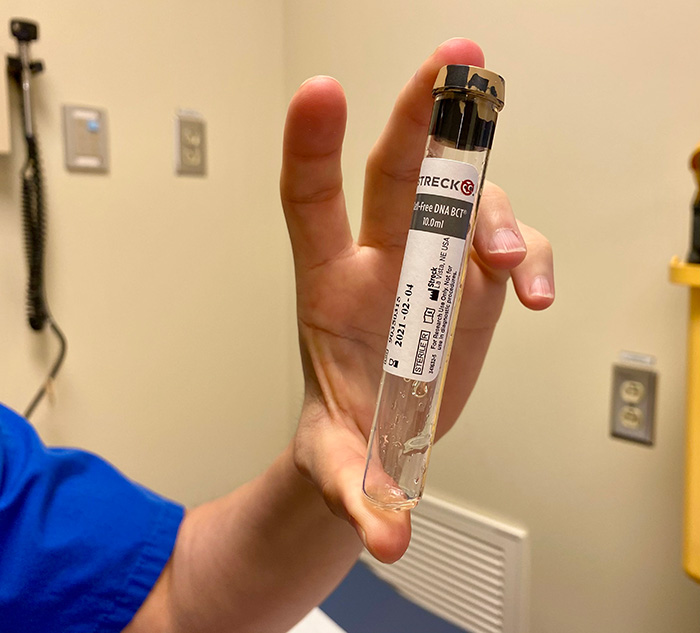
Stella Kozuszko, transplant nurse at the Ajmera Transplant Centre, (L), and Dr. Yas Moayedi, heart failure cardiologist at the Peter Munk Cardiac Centre, each hold a cell-free DNA test vial. They are both part of Meghan Wallace’s care team. (Photo: UHN)
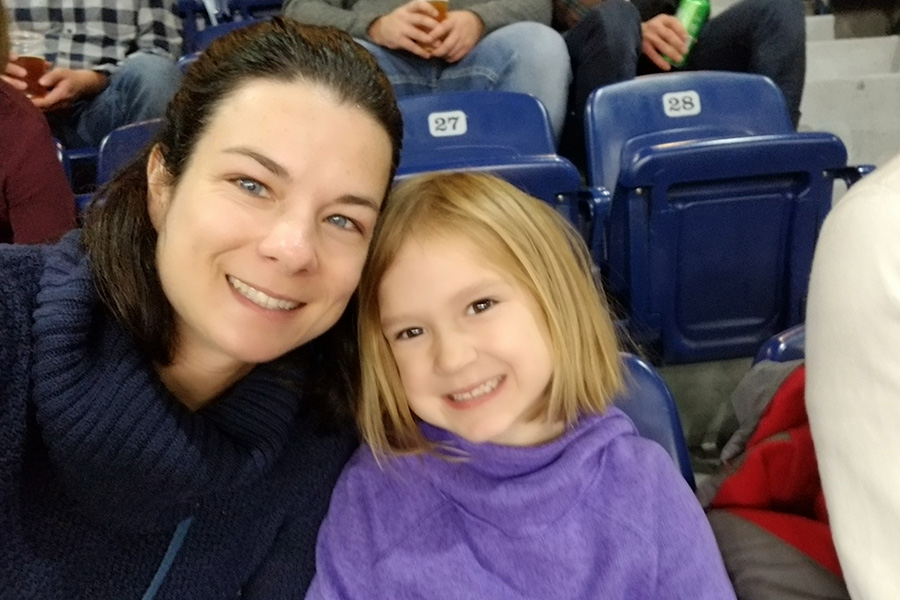
For heart transplant recipient Meghan Wallace, heart biopsies became an all-too familiar procedure in the days and months following her transplant.
And, over time, the procedure, which tells clinicians if her body is rejecting the new heart, became particularly risky for Meghan. Another biopsy could lead to permanent damage.
Using an innovative blood test, her care team at UHN’s Peter Munk Cardiac Centre (PMCC) designed an approach that’s just right for her – and today, Meghan hasn’t had a heart biopsy in more than two years.
“For me, a blood test is a thousand times better than getting a biopsy,” says Meghan, who received a new heart in 2015. She was diagnosed with dilated cardiomyopathy at age 12, causing her heart muscle to thin and enter early heart failure.
For heart transplant patients, biopsies are required on a weekly basis for the first month after their operation, twice monthly for the second month, and then monthly – up to 18 biopsies – on a specifically regimented schedule.
The traditional heart biopsy procedure involves a bioptome, a small pincher-shaped instrument inserted into the neck and guided to the heart, to obtain small tissue samples. In addition to evaluating rejection after a heart transplant, biopsies are also used to diagnose certain cardiac disorders such as amyloid or sarcoidosis.
Biopsies are a safe and reliable procedure for the majority of patients. But for some patients such as Meghan, the complication risk is higher – years of having a bioptome inserted through the neck can cause the skin and muscle to stiffen and scar. Meghan also has a clip on her tricuspid valve to prevent leakage, and a biopsy runs the risk of displacing it.
The alternative method is known as a liquid biopsy, a blood test which can detect levels of rejection in a transplant recipient. The most commonly used is gene expression profiling (GEP) but one flaw of this test has been exacerbated by the COVID-19 pandemic – if a patient has a viral infection, it can cause a false positive.
“It’s very frustrating for patients to have falsely positive tests, which lead to biopsies that are unnecessary,” says Dr. Yas Moayedi, cardiologist at the PMCC. “We are optimistic and excited about the potential alternative, the cell-free DNA test.“
Cell-free DNA (CfDNA), under brand names such as Allosure, analyzes the levels of donor DNA present in the transplant recipient’s bloodstream. If it’s below a certain percentage, there’s no rejection. If it’s above a certain threshold, rejection may be present – and only then will a patient go for a biopsy to evaluate further.
Unlike GEP, viral infections don’t affect the results of the CfDNA test. It also detects the two different forms of rejection, cellular and antibody, and can be performed at any blood clinic – saving the patient a trip to the hospital, especially during a pandemic.
“We’re on the brink of innovation – no other Canadian institution uses this type of liquid biopsy,” says Dr. Moayedi. “COVID-19 forced us to think outside the box.”
“For a few patients, we’ve averted biopsies that may have been unnecessary and with high complication rates – plus avoided the risks of coming to the hospital.”
Although Meghan isn’t a new transplant recipient, she required a biopsy earlier this year after a change in her immunosuppression medication. She also has Epstein-Barr Virus (EBV), a potentially dangerous virus for transplant recipients.
Meghan was an ideal candidate to try the CfDNA test.
“I think it’s amazing – it’s so much less invasive, and if it gives us the same information, then sign me up,” says Meghan. “For me, it’s a simple trip to the blood lab and no false positives – it’s a lot easier.”
Unfortunately, the CfDNA test is not covered by the province of Ontario, but Dr. Moayedi hopes to see the test become more available for patients and one day as standard of care for rejection surveillance.
“It’s reassuring for patients to know there’s another option,” says Dr. Moayedi. “One that’s just as adequate – and better for the patient’s quality of life.”
The Peter Munk Cardiac Centre’s Allosure cell-free DNA kits were donated by medical company CareDx for compassionate use.