Toronto General Hospital (TGH) – the only Canadian site – and nine centres in the United States are part of an ongoing U.S. Cystic Fibrosis Foundation consortium of leading academic transplant centres whose goal is to improve the lung transplant experience for people with cystic fibrosis (CF).
As part of the U.S. Cystic Fibrosis Foundation’s commitment to this goal, care teams from 18 blue-ribbon CF and transplant programs recently came to Toronto for a “benchmarking visit” to observe how TGH and St. Michael’s Hospital (SMH) work together to ensure CF patients are well cared for before and after their lung transplants to achieve outstanding results.
Cystic Fibrosis Canada is a dedicated supporter of the program at TGH.
Toronto was chosen for a visit due to its excellent transplant outcomes for CF patients, and strong culture of collaboration between the transplant and CF care teams.

Dr. Cecilia Chaparro
“What is unique for CF patients in Toronto is the strong communication between the two hospital teams, resulting in exceptional and comprehensive care for our patients,” says Dr. Cecilia Chaparro, the first respirologist to hold a joint appointment in the SMH Cystic Fibrosis Clinic and TGH’s Lung Transplant Program. “We identify issues and barriers early, and our patients trust us to work with them to identify the best solutions.”
Better patient outcomes
This teamwork between the two hospitals is paying off in terms of better patient outcomes.
Dr. Christian Merlo, Associate Professor of Medicine and Epidemiology at Johns Hopkins University School of Medicine in Baltimore, notes that TGH takes on some of the highest-risk patients, yet our outcomes are excellent. “We are very interested in adopting some of the strategies we saw here to improve allocation and (donor organ) survival in the U.S.,” Dr. Merlo says.
The probability of surviving one year after a lung transplant at TGH is about 90 per cent; at five years it’s about 70 per cent, both higher than U.S. rates.
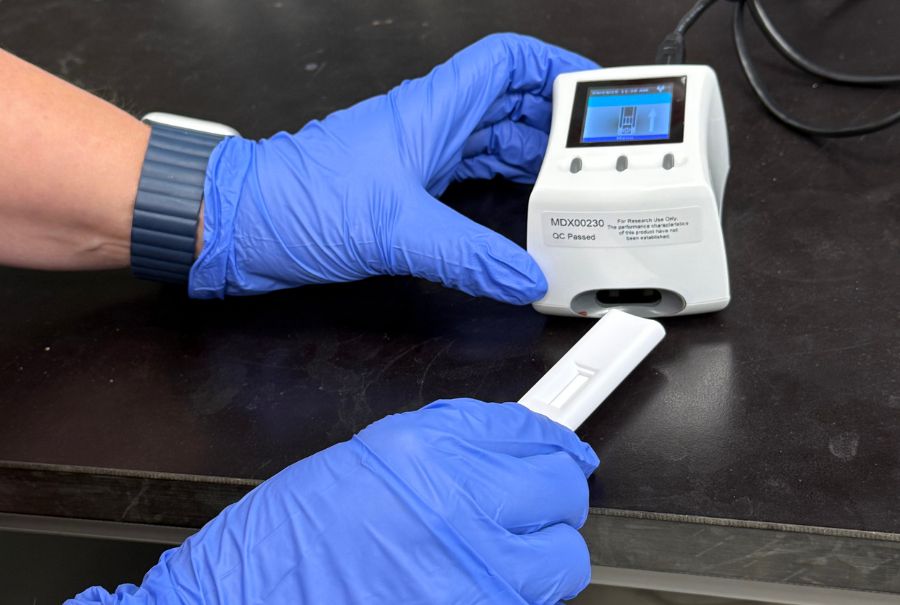
About one-third of all transplants at TGH involve the innovative Toronto Ex Vivo Lung Perfusion (EVLP) System. This technology was pioneered by a team led by Dr. Shaf Keshavjee at TGH in 2008 with the financial support of donors through Toronto General & Western Hospital Foundation. It can assess, improve and treat donor lungs, adding previously unusable lung into the donor pool, so many more are available for transplant. In just five years, EVLP has helped increase the number of lung transplants performed in Ontario by 70 per cent and improved outcomes.
Overall, Dr. Merlo was impressed with what he witnessed here.
“We saw how the teams in Toronto are on board to make the best decision for the patient,” he said. “It’s not just one person, everyone has a voice. Everyone’s opinion is listened to and respected. And everyone feels comfortable in voicing their opinion. That was awesome to watch.”