Registered nurse Maria Pyun of the Emergency Department at Toronto General Hospital demonstrates how to prepare a swab as part of a Panbio rapid test to determine if someone is presumptive positive for COVID-19. (Photo: UHN)
When the pandemic’s third wave made its way into UHN’s Emergency Departments (EDs), the ability to quickly screen and triage patients became increasingly critical.
“In some of the earlier waves, we’d get three or four patients a day that would be COVID-positive out of all the patients we tested,” says Debra Davies, Nurse Manager of the ED at Toronto General Hospital.
“But during the third wave, I remember one shift where we had eight positive patients and six of them needed admission.”
In March, just as the third wave arrived in Toronto, UHN’s ED nurses were trained and prepared to use a new rapid antigen testing kit that could produce a COVID-19 test result in just 15 minutes. That meant teams no longer had to wait eight to 12 hours for the lab-based polymerase chain reaction (PCR) test result to begin triaging COVID-positive patients.
Two dedicated teams from UHN’s Laboratory Medicine Program (LMP) and EDs worked tirelessly for months behind-the-scenes to bring this test to the bedside. LMP’s Point of Care team, led by manager Christine Cursio and clinical biochemist Dr. Davor Brinc, was tasked with validating the Panbio rapid antigen test in December 2020.
From January to March of this year, UHN staff performed hundreds of tests as part of the validation study and assessed the data in almost real-time. In symptomatic patients, the team observed a specificity of 99 per cent – when Panbio was positive, it was accurate 99 per cent of the time – and a sensitivity of 49 per cent – Panbio failed to pick up positive cases as identified by the nasopharyngeal (NP) swab and lab-based PCR testing, approximately half the time.
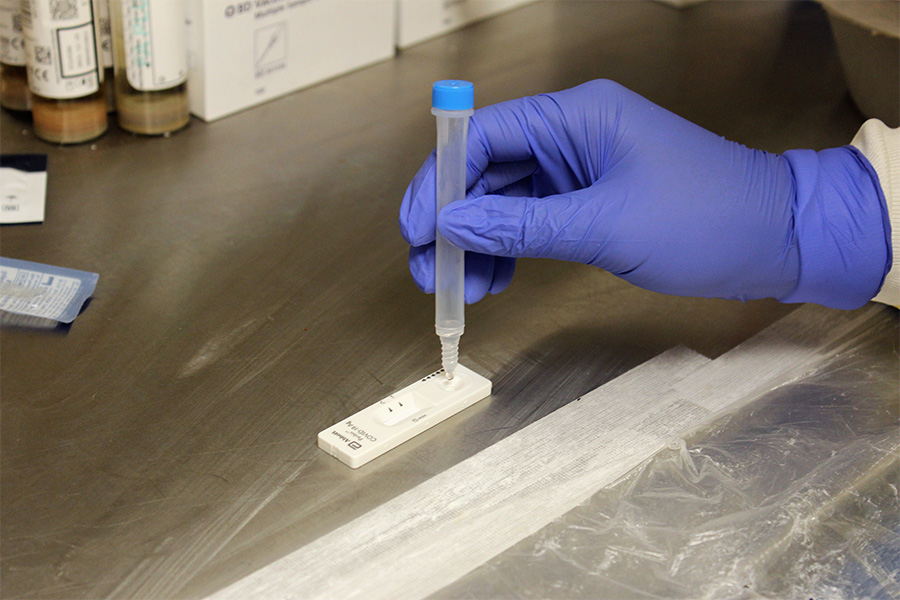
“We came up with the best-case scenario,” says Dr. Vathany Kulasingam, Division Head, Clinical Biochemistry, LMP. “Based on its performance during the validation study, the Abbott Panbio rapid test can be a screening test using a nasal swab that can be used in clinical decision making only if the result is positive.
“An NP swab must always be performed along with the Panbio rapid test and sent for lab-based RT-PCR testing,” Dr. Kulasingam continues. “The Panbio rapid test result is considered presumptive positive only but may be used as an effective tool for bed flow in the ED and for bed assignment on the inpatient units, while waiting for the Microbiology Lab-based RT-PCR result to be completed.”
In less than three months, the teams came together to develop a process for data collection, design standard operating procedures and train staff on this new point of care (POC) test.
“Having a positive Panbio COVID result can really help streamline the flow of the patients and identify their right bed on the COVID unit,” says Debra. “Our patients are often positive with symptoms like abdominal pain or a headache.
“Using the POC helped us get patients out of the hallway and into isolation quickly – mitigating risk.”
Helpful to isolate patients from congregate living settings who test positive
The Panbio tests have also been helpful for patients without a fixed address who cannot self-isolate in the shelter system.
“We don’t want to send a positive patient back out to these congregate settings where they’re putting a lot of other vulnerable people at risk,” says Debra.
A positive POC test allows ED staff to transfer these patients to the COVID recovery hotel quickly instead of waiting for the lab-based PCR test result in the ED.
At the peak of the third wave, UHN’s ED staff performed about 40 COVID tests per day – using the Panbio kits in approximately half of patients.
“Sadly, you can really see how much of a difference it’s making when you have more positive patients,” says Debra.
She applauds the LMP team for the outstanding work they do to support all of the efforts in the ED.
“Even though they don’t see all patients, we can’t do our job without the people in the lab – they are so much a part of the patient care we deliver down here and that’s important to know,” Debra says.
This small intervention looks to have big impact—one that helps test, triage and treat patients battling this deadly virus.
