Brad Pope was one of the first patient’s to use Medly. It’s helped him get back to normal. (Photos by Tim Fraser)
By Wendy Glauser
Brad Pope was having a fairly routine day at work when he suddenly felt short of breath. This was alarming for Pope, a 47-year-old avid cyclist from Toronto. “It felt like I was climbing at a high altitude, dealing with thin air, and couldn’t catch my breath,” he recalls.
He went to a walk-in clinic, where he was referred for an echocardiogram and a stress test. It was after those tests that Pope was given grim news: heart failure. “In that moment, all I could think was, ‘I’m dying,’” he says.
After his local hospital sent him to the Peter Munk Cardiac Centre, he came under the care of Dr. Heather Ross, Division Head of Cardiology at the Peter Munk Cardiac Centre, Site Lead for the Ted Rogers Centre for Heart Research, Loretta A. Rogers Heart Function Chair and Pfizer Chair in Cardiovascular Research, who told him some hopeful news – he would get on his bike again. Pope managed his condition with medication, but a year later had the first heart attack he could feel. Emergency room staff told him he had a 95 per cent blockage of the left anterior descending artery. “Things were pretty critical,” he says.
After having emergency surgery to remove the blockage, he was told by Dr. Ross that a new remote monitoring application called Medly would help manage his condition.
Identifying problems early
Dr. Ross, along with Dr. Joe Cafazzo, Executive Director of University Health Network’s eHealth Innovation and Wolfond Chair in Digital Health, developed and launched Medly in 2016. This tool is a heart failure monitoring platform that’s accessed through a mobile app. Patients enter daily metrics, such as their weight, blood pressure and heart rate, and that information is assessed by a rules-based in-app algorithm in real time. An actionable feedback message – normal, caution or critical – is sent to patients, and if there is any indication of deteriorating health, the patient’s care team can intervene quickly. Through remote monitoring, clinicians have access to continuous data, so treatment is not restricted to what is observed during hospital visits alone.
Pope eagerly agreed to be one of the first patients to use Medly. Every morning, he gets on his scale, slaps on his blood pressure cuff, checks his heart rate and records symptoms like fatigue or shortness of breath. “It gives me peace of mind,” he says. “My file isn’t forgotten until the next time I have an appointment, where they crack it open and say, ‘OK, where is he at?’”

Medly’s impact
The impetus behind Medly was to care for patients with heart failure every day, not just when they see their doctor. In the first year after a diagnosis, heart failure patients spend, on average, 27 days in hospital, often for what could be preventable issues, such as early signs of a possible heart incident or medications that need adjusting.
The past four years have made it clear that Medly is having the desired impact – and generating
excitement for its potential. Research from the Ted Rogers Centre for Heart Research at the Peter Munk Cardiac Centre has found that those who use Medly are rehospitalized with heart failure–related complications at half the rate of those who don’t use the platform. And when they do have to be hospitalized, they are staying an average of two days less. “Because of Medly, we’re catching issues before they become serious problems,” says Dr. Ross.
Mary O’Sullivan, a registered nurse and Lead Clinical Coordinator for Medly, oversees a small team of three nurse co-ordinators, who together monitor the 729 patients currently enrolled in the program. “Medly allows us to be in lockstep with the patient,” she explains. “And for a condition where a small deviation can lead to a life-threatening incident, being able to catch symptoms in real time makes a big difference.”
The future of Medly
Medly keeps evolving in significant ways. Dr. Ross and her team are adding video and asynchronous secure messaging, which will help physicians communicate faster and let them see whether their patients are showing worrying physical signs, such as swelling. They’re also bringing Medly to northern communities, including Moose Factory and Moosonee, Ont., with the hope that it can reduce disparities in health outcomes for Indigenous patients. “Our vision is access to equitable, high-quality care for all. The care you receive shouldn’t differ based on where you live in this country,” says Dr. Ross.
It’s essential for heart failure patients to receive the optimal therapeutic doses of heart failure medications. These medications need to be increased slowly and at regular intervals – and Medly helps people stay on track. According to the data, 91 per cent of patients who use the platform are achieving their optimal medication dose at six months, compared to 53 per cent for those who only visit the clinic in person. The time it takes to achieve dose optimization is also eight weeks less when conducted remotely.
Medly is integral to the care the Peter Munk Cardiac Centre has provided to heart failure patients during COVID-19 and has shown the potential for future remote monitoring opportunities. Since March 2020, 400 more people have been onboarded remotely to the program. “Because of Medly, we weren’t dependent on space in a clinic or doctor availability, and patients didn’t have to put themselves at risk by coming into the hospital,” says Dr. Ross.
As for Pope, Medly makes him feel less alone on his journey in managing a progressive disease that requires continuous vigilance. “It keeps me in check,” he explains. While it’s been a long road, Dr. Ross was right when she said Pope would get back on his bike. “I came so close to dying,” he says. “I can’t express how grateful I am.”
50% decrease in rehospitalizations among heart failure patients who used Medly compared to those who didn’t use the platform.
Source: Journal of Medical Internet Research
How it works
Medly is a revolutionary platform that’s transforming patient care. Every morning, patients input certain vitals, such as weight and blood pressure, which then get sent to the Peter Munk Cardiac Centre. If there’s a problem, the patient receives a call or an email. The idea is to keep care going at all times, not just at appointments with doctors.
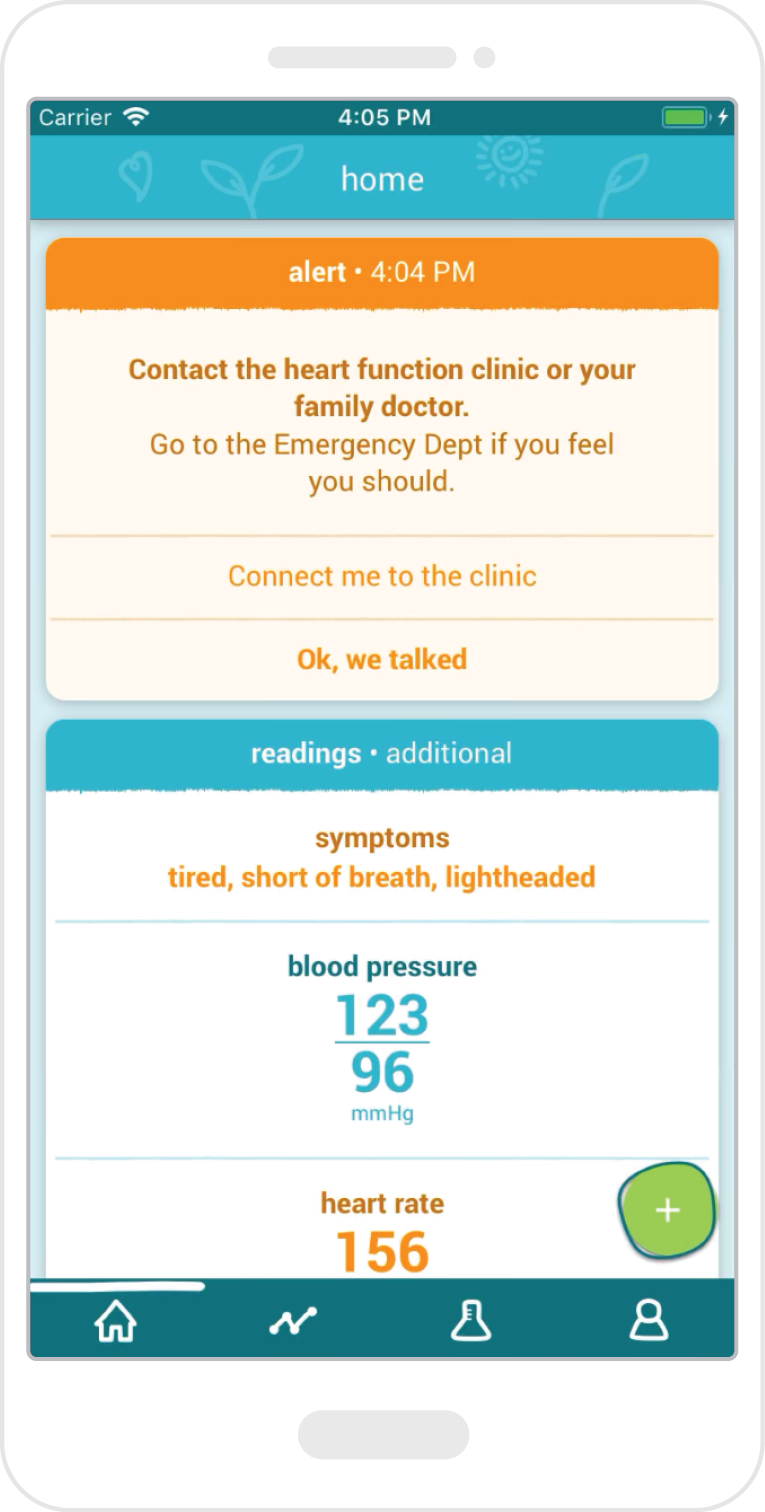
Receive alerts
An alert gets sent to the patient’s app if a concerning medical issue is identified.
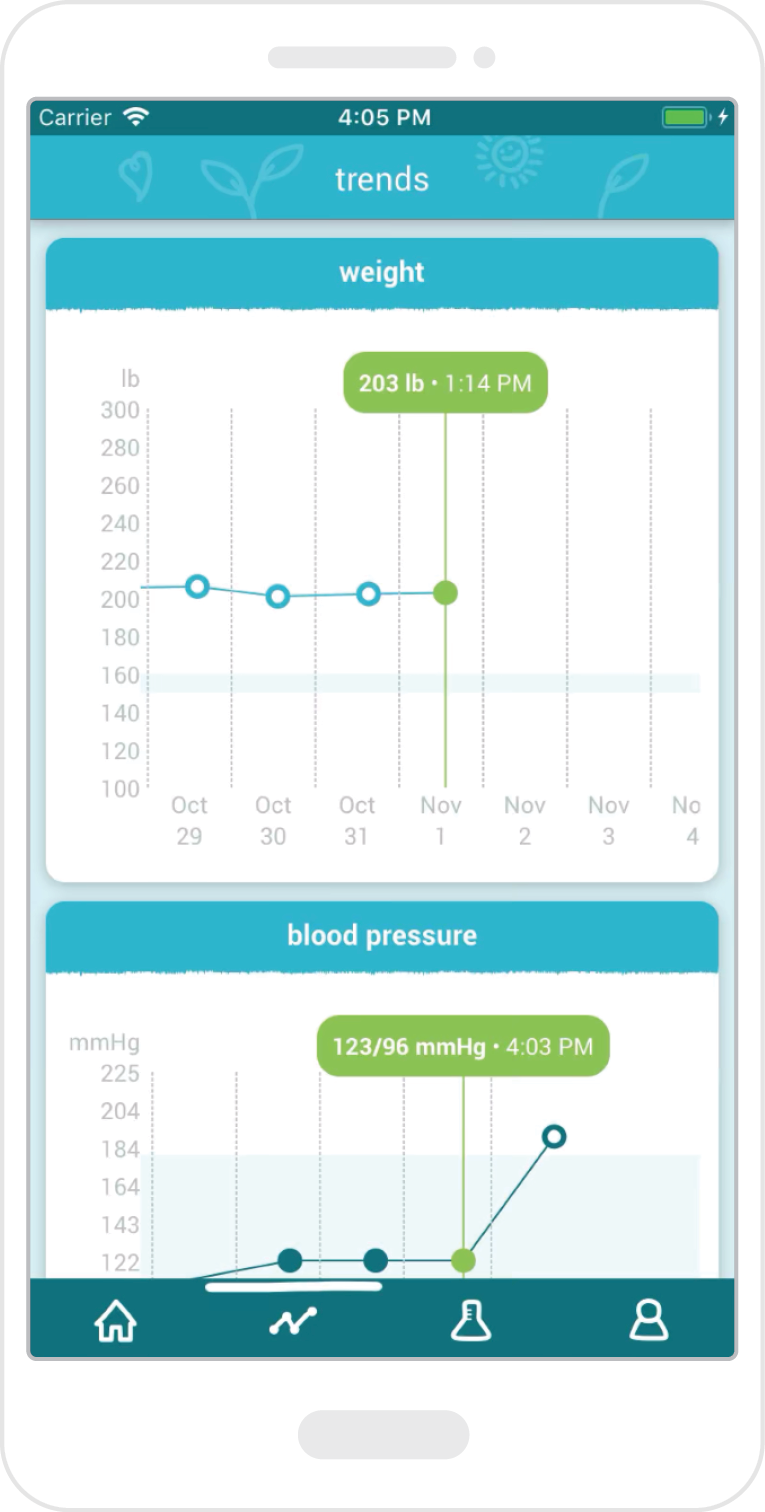
Track Vitals
The user-friendly display makes it easy to see weight or blood pressure changes.

Access results
The user-friendly display makes it easy to see weight or blood pressure changes.
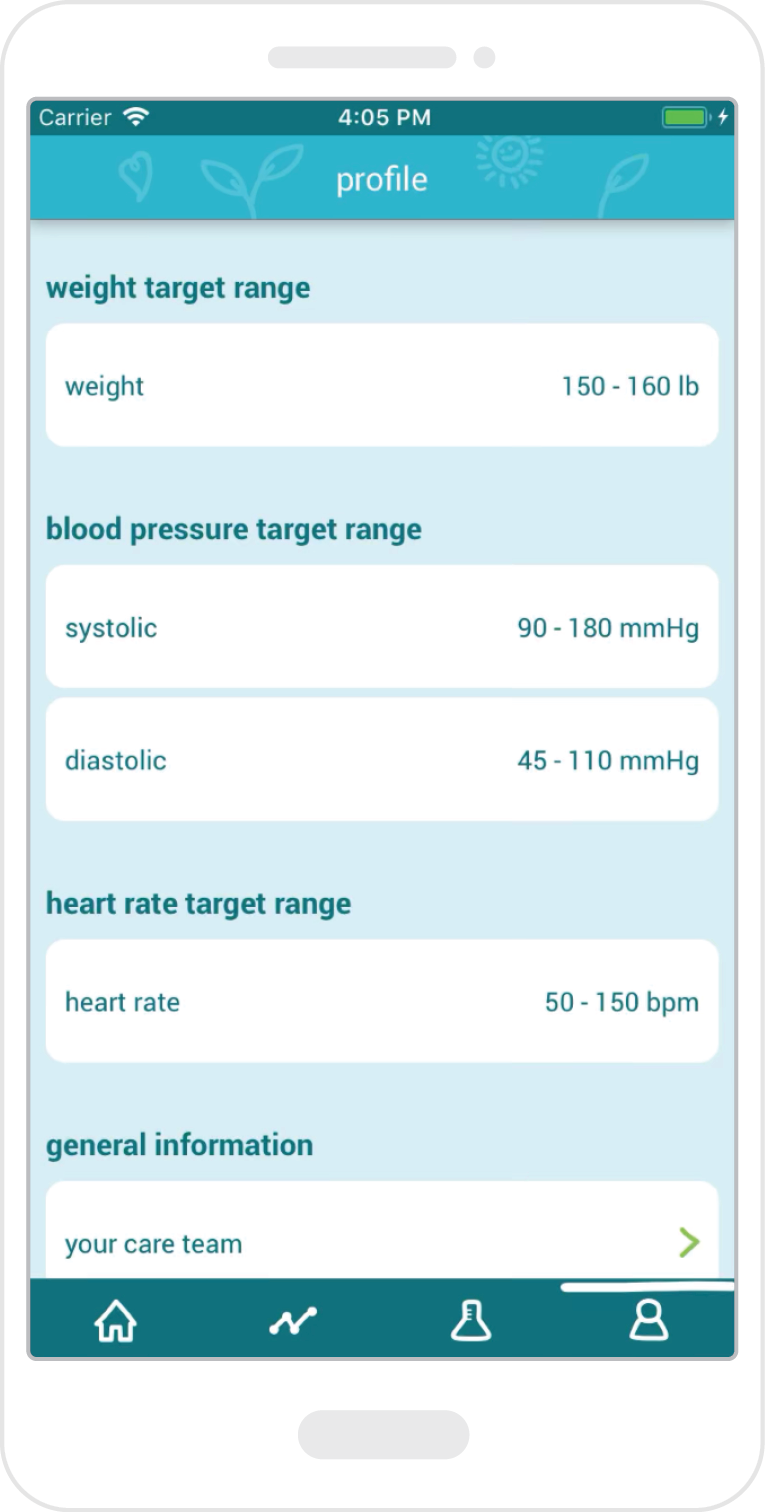
Follow targets
Users can see if their heart rate, weight and blood pressure targets are within range.
A partnership with Apple

In September 2020, the Ted Rogers Centre for Heart Research at the Peter Munk Cardiac Centre announced a historic new partnership with Apple to investigate whether physiological signals from the Apple Watch – such as heart rate and blood oxygen – could strengthen care in heart failure. Dr. Heather Ross and her team anticipate that continuous data derived from the Apple Watch will help identify issues with the heart even earlier and improve patient outcomes. The partnership is Apple’s first Canadian healthcare partnership and it’s the only cardiac partner globally. There is an unmet need for more widely available clinical assessment tools that proactively monitor and treat heart failure patients outside the hospital. Traditionally, clinicians rely on patient data gathered during a few in-person clinical appointments, which leaves room for important information that surfaces between these appointments to be missed. This study will help determine whether devices such as the Apple Watch could meet this need. “It’s a tremendous opportunity,” says Dr. Ross.
This article originally appeared in the 2021 Peter Munk Cardiac Centre annual report. Read it here.
