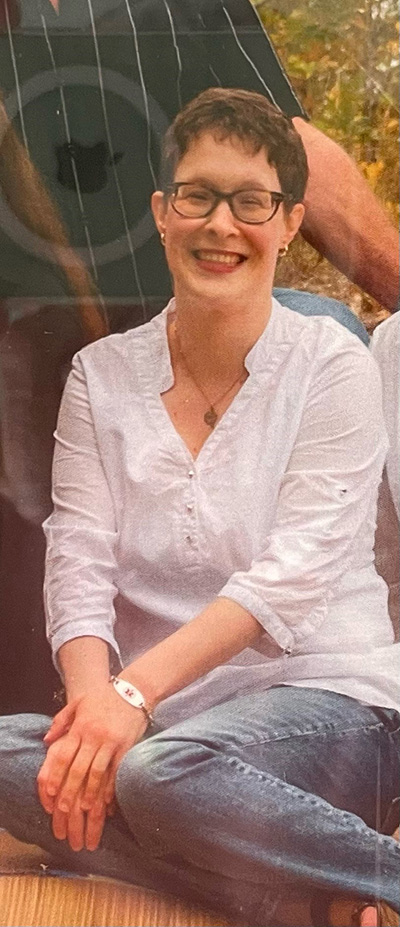
Dr. Mark Osten, Associate Director, Structural Heart Disease Intervention Program at UHN’s Peter Munk Cardiac Centre, was part of the team that determined patient Alex Hill needed a larger heart valve, which was only available via Health Canada special access. (Photo: UHN)
In 2019, doctors told Alex Hill she was in need of a heart valve replacement.
A then 31-year-old personal support worker (PSW) in Goderich, Ont. Alex waited patiently for the next step – before the pandemic brought everything to a standstill.
Alex was born with Tetralogy of Fallot (ToF), a congenital heart defect that occurs when a baby’s heart doesn’t form correctly in utero. Aside from undergoing open-heart surgery at the age of five, Alex remembers having a fairly normal childhood.
“I would get short of breath if I did intense physical activity,” she says. “But I could still go to gym class.
“I never really felt restricted.”
ToF didn’t stop Alex from enjoying school. An enthusiastic learner, Alex has two degrees – one in Fine Arts, the other in teaching – as well as a diploma in Early Childhood Education and a PSW certificate.
Like the rest of the world in March 2020, Alex struggled to cope with the changes brought on by the pandemic. As a PSW, she was further burdened by the fear that plagued the retirement home she worked in.
As a ToF patient in need of a new heart valve, she was devastated.
“I was exhausted all the time.” she recalls. “No matter how much I slept I woke up tired. I had chest pains and palpitations – symptoms I hadn’t experienced since I was a kid.
“I just kept wondering: when am I going to get this surgery?”
As the world breathed a sigh of relief with the vaccine rollout, Alex’s health anxiety was at a breaking point.
“My doctors had told me if the procedure was put off for too long, they wouldn’t be able to repair my heart. The damage would be irreversible.”
No other options but technology not approved by Health Canada
In March 2021, Alex met with Dr. Eric Horlick, Director of the Structural Heart Disease Intervention Program at University Health Network’s Peter Munk Cardiac Centre. Dr. Horlick and his team, including Dr. Mark Osten, Associate Director, Structural Heart Disease Intervention Program, determined that the readily available valves were too small for Alex.
“Without a larger valve, we couldn’t replace Alex’s pulmonary valve percutaneously,” explains Dr. Osten. “She would have to undergo open heart surgery for a second time in her life to get the replacement.”
The valve Alex needed was under Health Canada special access, a process that requires doctors to make an argument that their patient has no other options except a technology that has yet to be approved by the federal government department responsible for national health policy.
As her care team set to work on procuring her valve, Alex persevered at the retirement home, despite her declining health.
“I double-masked, I sanitized my hands. I tried to keep myself as safe as possible,” she says. “The place I worked at did a great job. There were no outbreaks, and I still haven’t had COVID. I feel very lucky in that respect.”
Procedure a success, positive change almost immediate
Finally, Alex received the good news: the valve had arrived.
Her procedure was scheduled for early September and, with her permission, would be live broadcast to the PICS-AICS (Pediatric and Adult Congenital Interventional Society) Conference in Chicago.
“PICS is the largest symposium specifically dedicated to congenital interventional procedures worldwide,” says Dr. Osten. “The symposium asks a few select hospitals worldwide with expertise in congenital heart disease to perform two live cases, and we chose this intervention specifically to highlight the technical challenge with this specific implant.
“It’s an opportunity to highlight what we do at UHN, and it’s a privilege that they choose us to perform the live cases. They have to have a lot of trust in our expertise. It’s live to an audience of over 2,000.”
The procedure was a success, and the change in Alex’s health was almost immediate.
“Three days after she returned home, I started noticing a nice colour in her face,” says Rose, Alex’s mom. “She has energy now, and each day she’s getting better and better.”
Just weeks after the replacement, Alex and Rose found themselves enjoying activities they hadn’t done together in years.
“We’re doing all kinds of things around Alex’s apartment,” Rose says. “We’re going out to dinner, to the movies. I’m getting to know this side of her that got lost when she was really sick.
“She’s positive, she’s happy.”
Just under a month post procedure, Alex is well on her way to physical and emotional recovery from the last three years.
“It’s been a long road, but I’m so incredibly grateful,” she says. “I’m grateful to all the nurses and staff who took care of me during my hospital stay.
“I’m grateful to Dr. Horlick and his team for this new lease on life.”
