Dianna Bois had an aortic aneurysm that was so complex it took a team to save her.
By Elizabeth Chorney-Booth
Dianna (Tracy) Bois often goes on walks, but there was one stroll in mid-2019 she’ll never forget. As the 70-year-old from Innisfil, Ont., was passing by a nearby lake, she began to feel light-headed. She quickly walked home, where her symptoms got worse. She soon started having trouble concentrating, but she was most concerned about the veins in her arms, which started to enlarge. While at an appointment with a local physician for an unrelated health issue, Bois asked about her veins and the doctor was concerned enough to send her for an MRI. Bois was shocked by the results: she was suffering from a potentially fatal aortic aneurysm.
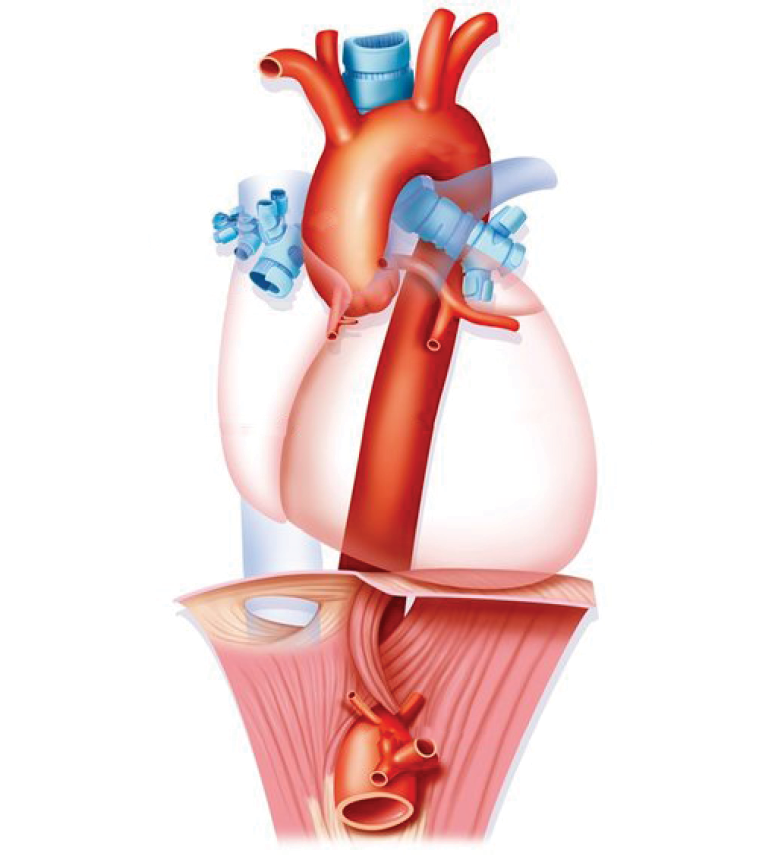
An aortic aneurysm is a bulge in the aorta (the artery that carries blood from the heart to the rest of the body) that can be fatal should it rupture. These aneurysms often don’t present symptoms until they’re quite significant – by the time Bois saw her physician, her aneurysm stretched from her heart down the entire length of her torso into her groin area, appearing as an elephant’s trunk wrapped around the largest blood vessel in the body.

Most aortic aneurysms aren’t difficult to treat, as they affect a small portion of the aorta, so clinicians at Bois’ nearby hospital thought they could easily take care of the problem. But once they realized the size and complexity of the aneurysm, which affected the entire length of the aorta from close to the heart to the leg vessels, including multiple branches to the brain and abdominal organs, they didn’t think they could safely perform surgery.
For this complex procedure, she was referred to Dr. Jennifer Chung, an aortic surgeon in the Peter Munk Cardiac Centre at University Health Network’s Sprott Department of Surgery. “I was discouraged, but once I met Dr. Chung I felt so confident in her,” says Bois. “She drew out exactly what was happening with my body like an artist, a Picasso. I had no doubt that she would be essential in getting me through this.”

Operating on the inoperable
How did Dr. Chung know she could operate? Because, along with her knowledge and experience, she works with an expert team of surgeons and imaging specialists to solve cases like Bois’, which are often too complex for most hospitals to tackle.
The surgeons, anesthesiologists, critical care specialists, nurses, imaging specialists and support staff at the Peter Munk Cardiac Centre are proud of their uniquely collaborative approach to patient care. In the spring of 2020, that philosophy was further boosted with the opening of its Thoracic Aortic Surgery Clinic. There, Dr. Chung and her colleagues – Dr. Maral Ouzounian, a cardiac and aortic surgeon in the Peter Munk Cardiac Centre at Sprott Surgery, and Antonia & Helga De Gasperis Chair in Clinical Trials and Outcomes Research; Dr. Thomas Lindsay, a vascular surgeon in the Peter Munk Cardiac Centre at Sprott Surgery; Dr. Kong Teng (K.T.) Tan, an interventional radiologist and Division Head of Medical Imaging at the Peter Munk Cardiac Centre; and the rest of their team – come together to work on some of the toughest aortic aneurysm cases that exist.
The new clinic was specifically created to treat patients suffering from aneurysms and dissections. All four clinicians were enlisted to address the complexity of Bois’ aneurysm and helped Dr. Chung with procedures that went beyond her specialized area of expertise. “What made her case so challenging was that it wasn’t just one part of the aorta being affected – it was all impacted,” explains Dr. Chung. “That can be quite daunting if you’re an expert in only one segment of the aorta. But because we work together and deal with everything from the valve right down to the legs, we felt quite comfortable with it.”

A new venue for collaboration
One of the advantages the new clinic has over other facilities is that it brings all of these various disciplines under one roof. Typically, a patient like Bois would have to make separate appointments to see cardiac surgeons who would address the portion of the aorta connected with her heart, and vascular surgeons who would deal with the vessels in the lower part of her body. The Thoracic Aortic Surgery Clinic brings all of those physicians together, which allows them to discuss cases and brainstorm approaches. This “three or four heads are better than one” approach allows clinicians to come up with comprehensive traditional and minimally invasive surgical solutions to save lives.
This was immensely beneficial to Bois, whose surgery affected such an expansive portion of her body. Dr. Tan provided crystal-clear images that allowed the surgeons to see exactly what was going on inside her and devise a plan of attack. The surgery began last spring, during the early days of the COVID-19 pandemic. The procedure started with the surgeons replacing the ascending aorta and arch, which is the part of the organ that bends up from the heart in a cane-like shape. This elephant trunk repair is a major surgery done only at specialized aortic centres and something Bois needed time to recover from before the team addressed the portion of her aorta that reached into her abdomen. In July, Bois returned to have her entire thoracic and abdominal aorta repaired. Bois is incredibly appreciative that the Peter Munk Cardiac Centre team provided such thoughtful care in such an unusual and stressful time, she says.
“It was a really extensive surgery,” says Dr. Ouzounian. “But after assessing her, we felt she was strong enough to undergo it. Because of the experience of our team, we didn’t feel like this was outside the realm of what we could handle.”
There are still many unanswered questions in the world of aortic surgery, and the clinic’s team-first process extends beyond the operating room, with all of the clinicians working together on several game-changing research projects. For example, Dr. Chung is interested in exploring why some people’s aortas may burst under the pressure of a relatively small aneurysm, while others’ will not. With cutting-edge radiologists, cardiologists and anesthesiologists at their disposal, the surgeons can test techniques other institutions can’t. “Innovation breeds innovation,” says Dr. Lindsay. “We’re at the stage where we can continue to evolve and improve, and really expand the horizons of how we treat aortic disease in Canada.”
A surgical success
While Bois’ kidneys were affected by the process – she had to undergo several months of dialysis during her recovery – she now feels renewed. She’s been spending as much quality time with her husband as she can and feeling appreciative about her ability to enjoy life again.
The aortic team’s confidence, camaraderie and thoughtful bedside manner made Bois feel truly cared for, and she is very grateful. But while her surgery was complex, it’s not unlike others the aortic team sees over the course of a year. The new clinic will allow countless other people like Bois to have another chance at life. “They are my heroes,” she says about the team that helped her. “They have a genuine caring concern and so much respect for one another.”
Interventions needed
80% people die after after their aneursym ruptures. Source: University Health Network.
Understanding Bois’ aneurysm
Bois’ aneurysm began in the ascending arch of her aorta and descended down the full length of her torso.
This article originally appeared in the 2021 Peter Munk Cardiac Centre annual report. Read it here.
Photos by Tim Fraser.


