Lindsay Bongard-Batori still remembers the frustration and sadness she felt as the slow advance of Alzheimer’s disease took away what should have been some of the best years of her mother’s life.
“My mom, Barbara, was my person – nothing explains it better than that,” she says. “She loved going for long walks and just appreciating the little things in life.”
As time passed, that began to change.
“She started repeating herself a lot,” Lindsay says. “Then, she started forgetting things.
“I remember one day she called me, crying. She had gone to the grocery store and couldn’t find her car even though the parking lot wasn’t that big. She was hysterical, and I had to talk her through it. We decided as a family, with her involved, that it was time to talk to her doctor.”
Those discussions eventually led to a diagnosis: Barbara was suffering from mild cognitive impairment, a common precursor to Alzheimer’s disease. Not long after, she suffered a frightening fall, which led her daughter to find a place that could provide additional care.
It was a painful time for Lindsay and her family.
“They say with Alzheimer’s, you mourn twice, and I understood right then what that meant,” she says.
Novel thinking, new theories
It’s estimated that more than 1.7 million Canadians will be living with Alzheimer’s disease by 2050, three times the current number, according to the Alzheimer Society of Canada.
Factor in the one million or so care partners needed to support this unprecedented increase, and the sheer volume of Canadians whose lives may one day be upended by the disease is staggering.
“These numbers are a wake-up call for our system – we can’t keep going the way we are,” notes Dr. Donald Weaver, a Senior Scientist at UHN’s Krembil Brain Institute and the Krembil Chair in Drug Discovery Research for Alzheimer’s Disease at UHN.
To Dr. Weaver, that means thinking outside the box, even if it raises questions about everything we think we know about the disease.
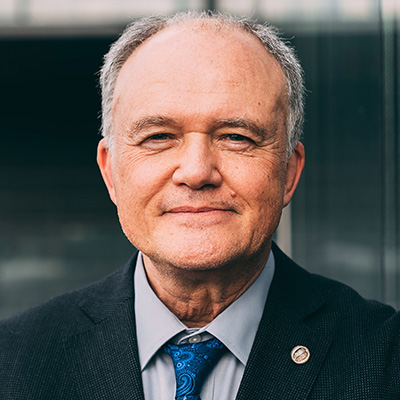
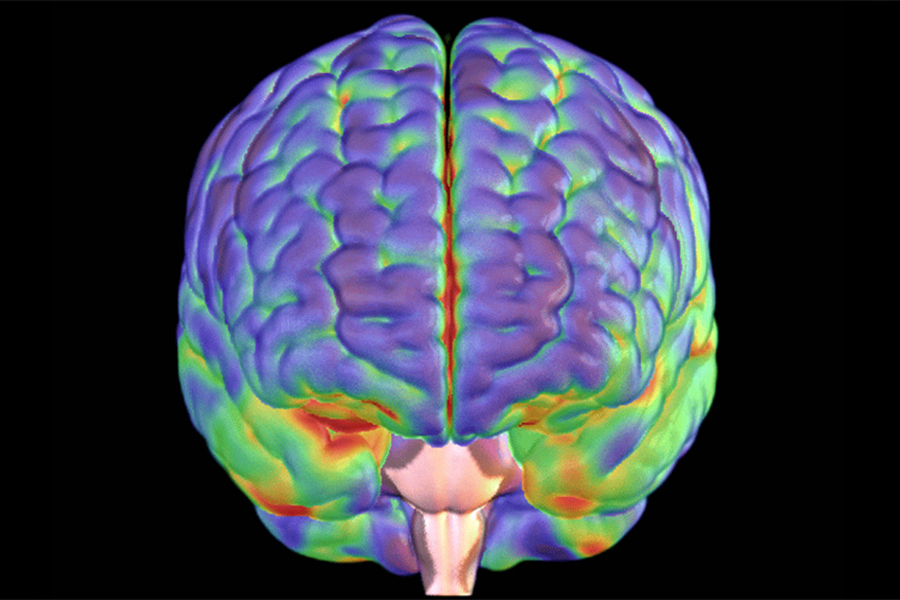
Dr. Weaver has come up with a novel theory as to why Alzheimer’s develops: it may be an autoimmune disease that attacks the brain. The idea challenges the prevailing view, which contends that the buildup of a peptide called beta amyloid in the brain is a key factor in the development of the disease.
“We’re arguing that amyloid is, in fact, a normal part of your brain,” Dr. Weaver explains. “It’s part of the immune system in your brain. It’s supposed to be there.
“The second notion our theory is based on is that, unfortunately, the immune system in your brain cannot differentiate between a neuron, which is a brain cell, and bacteria, which is an invading pathogen.”
This means that when your brain’s immune system is activated, be it by head trauma, excessive air pollution or an infection – at any point in one’s life – the beta amyloid that is sent to help may actually attack the very neurons it is trying to protect.
“As those brain cells are killed, they release their products as they fall apart,” Dr. Weaver says. “That turns on more inflammation, and this becomes a vicious cycle that goes on for decades and decades.
“The brain is just so crucial,” he adds. “It’s so complicated, and that’s why the idea of an autoimmune disease of the brain – which is what we are proposing – is so devastating.”
Future drug discoveries
The implications of this theory are enormous. If the factors that lead to Alzheimer’s disease accumulate from an early age, potentially even from childhood, they need to be taken much more seriously, says Dr. Weaver, adding that finding this new theory was a “eureka moment” in his lab.
It’s also “the most exciting time of my life,” he says, “because this is an opportunity for us to make drugs that address a target that we’ve discovered ourselves and targets that we think are the fundamental, underlying cause of Alzheimer’s disease.”
That’s exactly what Lindsay Bongard-Batori and the many others living with the impacts of Alzheimer’s and dementia want to hear.
“It makes me angry that there isn’t a cure yet,” she says. “But I hope in my lifetime that I get to see some progression. We hope it’s coming.”
10 Warning signs of dementia
1. Memory changes that affect day-to-day abilities
2. Difficulty doing familiar tasks
3. Changes in language and communication
4. Disorientation in time and place
5. Impaired judgment
6. Problems with abstract thinking
7. Misplacing things
8. Changes in mood, personality and behaviour
9. Loss of initiative
10. Challenges understanding visual and spatial information
*Source: Alzheimer Society of Canada