“Identifying family history paired with a robust genetic test can give us an insight into how a specific IRD will progress so that we can develop a care plan for the individual and potentially identify novel therapeutics for their specific condition,” says Dr. Brian Ballios, a clinician investigator at the Donald K. Johnson Eye Institute at UHN. (Photo: UHN)
Dr. Brian Ballios has a vision.
The clinician investigator at the Donald K. Johnson Eye Institute at University Health Network (UHN) and his team of specialists are moving towards a model of “same day care.” Their goal is for individuals referred to his clinic for an inherited retinal disease (IRD) – a degenerative genetic visual disease – to receive diagnostic testing, complete specialized imaging of the retina, and begin genetic testing all in one day.
“We’re approaching IRDs holistically to help my patients and their families find correct diagnoses and provide a detailed care plan to their local health care providers so we can co-manage their condition,” explains Dr. Ballios.
Many of Dr. Ballios’ patients are from out of town, since UHN is home to the only adult-specific IRD clinic in Ontario. Having an open line of communication between their family doctor and the specialist will allow their care to be managed locally, saving them from lengthy trips and additional costs to their care.
“Living with an IRD for more than 25 years is challenging, but the world-class team of ophthalmologists and scientists at UHN are on the forefront of research,” says Donna Green, a patient of Dr. Ballios, who lives with retinitis pigmentosa, a type of IRD. “They keep my family health team informed so that they can continue to be an active part in my care.”
IRDs cost Canadians about $1.6 billion annually. Two-thirds of that cost is borne by the affected individuals and their families due to a reduction in quality of life.
IRDs are a group of genetic diseases where one or more genes are not working properly, leading to visual impairments. In the case of retinitis pigmentosa (RP), more than 100 genes affect photoreceptors – the light sensing cells in the eye – causing them to progressively degenerate.
RP can first appear in childhood or as an adult, initially leading to a loss of night vision and side vision, and later can affect the central vision. Central vision is important for tasks such as reading, driving, and recognizing faces.
“IRDs are particularly challenging diagnoses to make since we need unique tools and tests to diagnose them,” explains Dr. Ballios.
Using specialized tools in Dr. Ballios’ practice, his care team can determine the health of the retina and surrounding structures in the eye. However, genetic testing for IRDs, which is approved under the provincial health plan, is one of the most important tools to determine the specific genes involved in an IRD.
“Identifying family history paired with a robust genetic test can give us an insight into how a specific IRD will progress so that we can develop a care plan for the individual and potentially identify novel therapeutics for their specific condition,” says Dr. Ballios.
Clinical care meets research
Dr. Ballios’ research benefits from his clinical practice where his patients’ diagnoses, perspectives and concerns can inform his research goals.
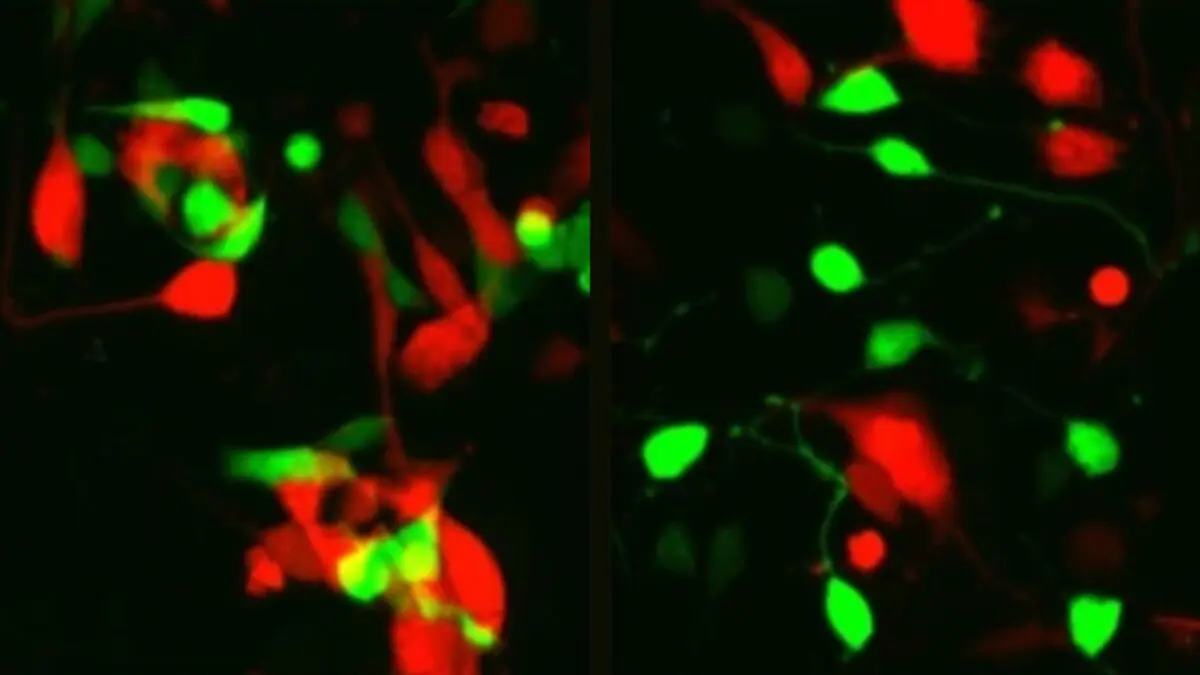
While there is an approved gene therapy for one genetic form of RP, it is not currently funded by provincial health plans, and it could potentially cost close to $1 million. Dr. Ballios is looking to use stem-cell therapies to identify treatments for these genetic blinding eye diseases.
While gene therapy requires functional cells of the retina, stem-cell therapies look to rebuild the retina, even if the cells have died.
“Stem cell therapy is promising, it’s a newer field than gene therapy or drug therapy but it has the potential to restore and regenerate vision that has been lost,” says Dr. Ballios.
The team at the Donald K. Johnson Eye Institute have strong clinical experience which pairs well with the already well-established basic science research programs, creating a centre of excellence for visual diseases like IRD.
“We’re truly fortunate to have a unique skillset across our scientists, clinicians and staff, which allows us to approach developing diagnostic tools and therapies for IRDs and other visual diseases in numerous ways,” says Dr. Valerie Wallace, co-Director of the Institute.
Those sentiments are echoed by Dr. Philippe Monnier, Senior Scientist at the Institute.
“Brian and I both have an interest in IRDs, it’s truly special to collaborate with him because he provides his clinical expertise, while I can inform him on what’s happening at the cellular level in some of these diseases,” says Dr. Monnier, who recently found a protein that has an influence on photoreceptor cell death.
Dr. Ballios says there is plenty of potential in the field of retinal diseases.
“I want to be able to provide a clear path for patients to navigate, and new therapies when there have been no choices previously,” he says.