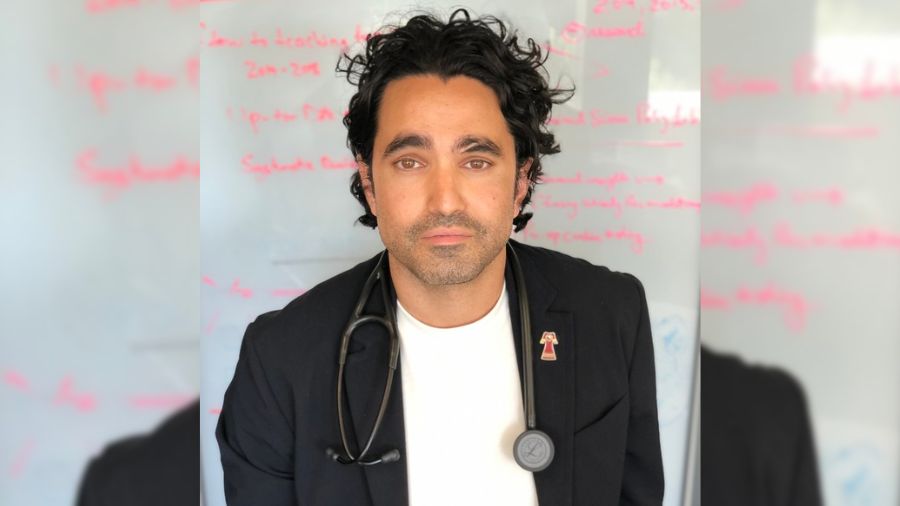
(L to R) Dr. Tom MacMillan consults with clinical nurse specialists Naudea Mair and Sherele McGhie. (Photo: UHN)
Dr. Tom MacMillan remembers feeling a combination of nerves and anticipation.
The general internist was taking part in leading a massive outpatient clinic refresh at the G. Raymond Chang Complex Medicine Teaching Clinic, aimed at serving an increasing patient demand across University Health Network, but still wondered if the patients would come.
“It was like when you plan a big party and you’re worried no one will show up,” Dr. MacMillan says, almost laughing in retrospect.
That was seven years ago. Now, patients have not only come, but the clinic, which is located in Toronto Western Hospital, has established itself as a critical pillar of general internal medicine (GIM) care.
The 2016 model was so successful – patient visits have steadily grown by about 300 per cent since the initial expansion – that they are now embarking on another expansion.
“We essentially became victims of our success,” says Dr. MacMillan, who is leading the project alongside his clinic co-lead, Dr. Tarek Abdelhalim.
A host of factors led to the clinic reaching capacity, including heightened awareness of the clinic throughout the hospital and in the community, as well as overall increased demand for health care.
“Being able to provide the best care we can during the pandemic has been the most rewarding part of working here,” says Sherele McGhie, a clinical nurse specialist (CNS) in the clinic.
“While most wound care clinics and general practitioners were unable to provide wound care, the Skin and Soft Tissue Infection Clinic opened its doors to provide this needed service.”
Reducing hospital admissions
Alongside patient care, a key driver of the original expansion was its goal to keep patients out of the hospital, a feat Dr. MacMillan says has been successful.
Through the Rapid Referral Program, appointments are set up for patients before they leave the Emergency Department (ED).
“I can send a patient home with the guarantee that they will have a follow-up in the coming days,” says Dr. Erin O’Connor, Deputy Medical Director of the ED at UHN.
The collaborative effort of GIM and ED has not only alleviated hospital admissions, but has also reduced the number of patients returning to the ED for follow-up care.
In its current expansion, the program will open the door to referrals from Toronto General Hospital’s ED, increasing access to outpatient care. Increasing the ability to care for this patient population within the clinic will contribute to decreased hospital admissions and reduced re-admission rates.
“Our patients have such diverse needs,” says Naudea Mair, a CNS at the clinic.
The clinic’s services range from wound care to hypertension to post-COVID care, treating patients with multi-system diseases and complex conditions.
“When a patient comes in with a skin infection, we don’t just look at the wound,” Naudea says. “We have to look at the whole patient and the whole picture.”
‘It felt like every other door was closed but the clinic’s door was open’
For patients who have been previously admitted to the GIM inpatient unit, the clinic also acts as a means for post-discharge care. The ability to refer patients for this purpose may assist in facilitating a safe discharge earlier than previously possible and prevent re-admission to hospital.
The “continuum of care” is incredibly reflective in the clinic, Naudea says. The physicians and nurses who staff the clinic also practice medicine in the in-patient setting, which instills confidence in patients who interact closely with their medical team.
This trust became especially important throughout the peaks of the pandemic as many patients sought out care through the clinic as a more comfortable alternative.
“Patients were glad that we were here at the beginning of the pandemic,” Naudea says. “We kept hearing from patients that it felt like every other door was closed, but the clinic’s door was open.”
The expansion will see the nursing and physician resources double, and will integrate additional Allied Health professionals such as pharmacists, social workers, and dieticians. It will roll out on a continuing basis as the team determines what works best for the clinic and for its patients.
“GIM involves a lot of logistical problem-solving and conversations with patients,” says Dr. MacMillan. “Learning how to best integrate new staff and processes will be based on the same things.”