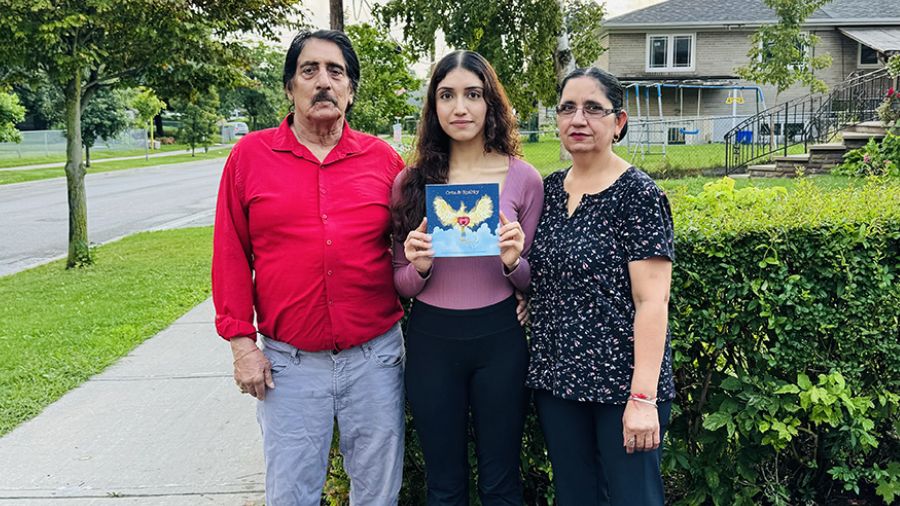
Emily Fox (L) | Age: 35 | Born: Windsor | Heart disease: Mitral valve prolapse | Diagnosed: June 2018 | Treatment: Medication
Katie Shea (R) | Age: 42 | Born: Ottawa | Heart disease: Dilated cardiomyopathy | Diagnosed: November 2018 | Treatment: Defibrillator implant and medication
(Photo by Tim Fraser)
Emily Fox and Katie Shea have a lot in common. They’re young, hardworking and active – and they also both have heart disease. On the outside, they’re strikingly similar, but on the inside, at the very cellular level, they are completely different.
These differences matter. Right now, two people could arrive at the hospital and get diagnosed with heart disease, yet one might respond well to treatment, while the other does not. One person could be discharged from the hospital the next day, while the other, despite receiving the same treatment, could require immediate transfer to the intensive care unit and die within days. “It’s hard to understand why patients respond so differently to the same treatment,” says Dr. Phyllis Billia, Director of Research at the Peter Munk Cardiac Centre.
Fortunately, the Centre is conducting crucial research that will one day allow doctors to use a patient’s unique genetic composition to dictate what treatment they receive. It’s called precision medicine, a term that has been around the medical community for a decade, but it’s at the Peter Munk Cardiac Centre where meaningful progress is being made.
According to Dr. Billia, precision medicine will help us answer many of the most pressing, and still unsolved, medical questions. This approach, which includes metabolomics, proteomics, transcriptomics and whole gene sequencing, will allow scientists to better understand the unique characteristics of every individual patient. As Co-Director of the Peter Munk Cardiac Centre biobank, Dr. Billia has overseen the acquisition of 150,000 patient blood and tissue samples – samples that will allow doctors to map human disease.
This information, combined with the power of artificial intelligence (AI) and machine learning, will help the team at the Peter Munk Cardiac Centre better decide how to treat two patients who may seem similar, like Fox and Shea, but who might need to be administered very different treatments in order to see the best outcome.
The potential for precision medicine to dramatically redefine a patient’s journey is massive, yet it’s also expensive. The Peter Munk Cardiac Centre is currently conducting 23 precision medicine–related projects, but researchers would like to be doing this with every patient. “To say it’s an ambitious and expensive goal would be an understatement,” explains Dr. Billia. “Yet we’re making progress every day.”
A PERSONALIZED APPROACH
In 2018, Shea was diagnosed with dilated cardiomyopathy, a condition that decreases the heart’s ability to pump due to an enlarged and weakened left ventricle. Fox has an arrhythmia, which causes the heart to beat abnormally fast. Both diseases are frightening and can be fatal if not treated properly.
When mapping out the optimal treatment plan for patients, clinicians apply past experience, available research, knowledge and intuition to generate the best possible outcomes. However, the majority of heart-related research has been on older white men, and while everyone’s physiology is similar, everything from diet to ethnicity to a family’s medical history can impact the way a person responds to treatment.
Whether it’s a young Black man or an older Indigenous woman, the medical field tends to take a “one-treatment-fits-all” approach. “That’s a problem,” explains Dr. Heather Ross, Division Head of Cardiology at the Peter Munk Cardiac Centre, site lead for the Ted Rogers Centre for Heart Research, Loretta A. Rogers Platinum Chair in Heart Function and Pfizer Chair in Cardiovascular Research. “As a patient, you want to know the therapy you’re receiving is based on evidence that’s relevant to you, so you can have greater confidence it will work. Unfortunately, so many of the studies clinicians refer to don’t reflect the individual in front of us.”
This is why, along with the focus on precision medicine research, the Peter Munk Cardiac Centre is working on what’s called personalized medicine, an area of medicine that takes into account patient differences outside of genetics, such as age, sex and ethnicity.
For Fox and Shea, that means considering how a 40-year-old woman’s response to treatment might differ from that of a 60-year-old man. Through personalized medicine, doctors will be better equipped to know why person A metabolizes medicine differently than person B, and prescribe two distinct treatments for the same disease. The more patients can be seen as individuals and the more specific research that is generated, the more likely people will experience improved long-term outcomes.
DIGGING INTO DATA
For someone working in one of the most multicultural cities in the world, the lack of information on diverse patients has frustrated Dr. Ross. Her drive to challenge the status quo led her team to create a specialized “data lake” — a computer platform that collects and stores a massive amount of patient information gathered from labs, pathology, radiology, echocardiography, electronic medical records, and more. It currently has 1.6 billion data points from two million patients, with 315,000 new pieces of information going into the system every day.
The data lake, which was generously supported by The Peter and Melanie Munk Charitable Foundation and The Rogers Foundation, is essential to making personalized medicine at the Peter Munk Cardiac Centre a reality. “We want to confidently say that based on the data in front of us, in the last 100 Black women between the ages of 40 to 50 we treated, we saw this happen,” explains Dr. Ross.
The sheer volume of data and time-sensitive nature of treatment makes it extraordinarily difficult for doctors to interpret this data on their own. As such, the Peter Munk Cardiac Centre is using AI to analyze the data and uncover patterns the human brain can’t see. “With the help of AI, we can design a specific treatment plan and create diagnosis models tailored toward an individual patient,” says Bo Wang, lead for the Peter Munk Cardiac Centre’s AI program.
As more data gets integrated, this infrastructure can recommend medicines or therapies doctors might not have considered before. “It’s an iterative process,” notes Wang. “We can validate new findings or confirm what people already know.”
With research that continues to challenge convention, the Peter Munk Cardiac Centre aims to one day fully incorporate the use of both personalized and precision medicine into a patient’s care plan. Personalized medicine will focus on a patient’s environment and characteristics such as age, sex and ethnicity, while precision medicine will focus on their unique genetic composition. “It will be tremendous,” says Dr. Ross, envisioning how patient outcomes will change with these new approaches.
For Fox and Shea, this means greater certainty in their lives. “Treatment applicable to everyone or specific treatment designed for me alone?” Fox asks. “The choice is clear”.
This article originally appeared in the 2020 Peter Munk Cardiac Centre annual report. Read it here.